Circumcision and HIV
[1][2] In 2020, the World Health Organization (WHO) reiterated that male circumcision is an efficacious intervention for HIV prevention if carried out by medical professionals under safe conditions.
[3][5] As of 2020[update], past research has shown that circumcision reduces the risk of HIV infection in heterosexual men, although these studies have had limitations.
Furthermore, WHO stated that: "While circumcision reduces a man’s individual lifetime HIV risk, the indirect effect of preventing further HIV transmissions to women, their babies (vertical transmission) and from women to other men has an even greater impact on the population incidence, particularly for circumcisions performed at younger ages (under age 25 years).
Male circumcision should never replace other known effective prevention methods and should always be considered as part of a comprehensive prevention package, which includes correct and consistent use of male or female condoms, reduction in the number of sexual partners, delaying the onset of sexual relations, and HIV testing, counseling, and treatment.In the United States, the American Academy of Pediatrics (AAP) led a 2012 task force which included the American Academy of Family Physicians (AAFP), the American College of Obstetricians and Gynecologists (ACOG), and the Centers for Disease Control (CDC).
[16][17] Aaron J. Fink several months later also proposed that circumcision could have a preventive role when the New England Journal of Medicine published his letter, "A possible explanation for heterosexual male infection with AIDS," in October, 1986.
[19] A meta-analysis conducted by researchers at the London School of Hygiene & Tropical Medicine examined 27 studies of circumcision and HIV in sub-Saharan Africa and concluded that these showed circumcision to be "associated with a significantly reduced risk of HIV infection" that could form part of a useful public health strategy.
The authors stated that three randomized controlled trials then underway in Africa would provide "essential evidence" about the effects of circumcision on preventing HIV.
[21] Experimental evidence was needed to establish a causal relationship, so three randomized controlled trials (RCT) were commissioned as a means to reduce the effect of any confounding factors.
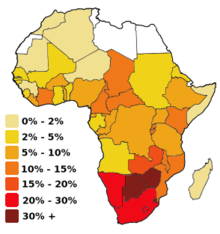
[26][27] Studies were conducted to assess the acceptability of promoting circumcision; in 2007, country consultations and planning to scale up male circumcision programmes took place in Botswana, Eswatini, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, Uganda, Tanzania, Zambia and Zimbabwe.
[28] In 2011, UNAIDS prioritized 15 high HIV prevalence countries in eastern and southern Africa, with a goal of circumcising 80% of men (20.8 million) by the end of 2016.
[29] As of 2020, WHO estimated that 250,000 HIV infections have been averted by the 23 million circumcisions conducted in the 15 priority countries of eastern and southern Africa.