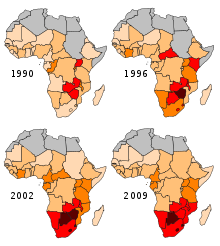
HIV/AIDS in Africa
Countries including Botswana, Lesotho, Malawi, Mozambique, Namibia, South Africa, Eswatini, Zambia, and Zimbabwe exhibit adult prevalence rates exceeding 10%.
[6] Efforts to combat the epidemic have focused on multiple strategies, including the widespread distribution of antiretroviral therapy (ART), which has substantially improved the quality of life and reduced mortality for those living with HIV.
[10] Despite progress, gender inequalities exacerbate the epidemic's impact, with young women in sub-Saharan Africa experiencing HIV infection rates three times higher than their male counterparts.
The most obvious effect ... has been illness and death, but the impact ... has ... not been confined to the health sector; households, schools, workplaces and economies have also been badly affected.
This group now accounts for 60% of all deaths in sub-Saharan Africa.... AIDS is hitting adults in their most economically productive years and removing the very people who could be responding to the crisis.
[12]The earliest known cases of human HIV infection were in western equatorial Africa, probably in southeastern Cameroon where groups of the central common chimpanzee live.
[20] The first epidemic of HIV/AIDS is believed to have occurred in Kinshasa in the 1970s, signaled by a surge in opportunistic infections such as cryptococcal meningitis, Kaposi's sarcoma, tuberculosis, and pneumonia.
[23] In the late 1980s, international development agencies regarded AIDS control as a technical medical problem rather than one involving all areas of economic and social life.
Because public health authorities perceived AIDS to be an urban phenomenon associated with prostitution, they believed that the majority of Africans who lived in "traditional" rural areas would be spared.
"In a normatively HIV/AIDS-stigmatizing Sub Saharan African communities, this suspicion of one's status by others is also applicable to individuals who are not HIV positive, but who may wish to utilize healthcare services for preventive purposes.
Well-designed programs are carefully tailored to national and local needs and conditions; focus resources on the mix of programmatic and policy actions required to address both immediate risks and underlying vulnerability; and are thoughtfully planned and managed to operate synergistically and consistently on multiple levels (e.g. individual, relationship, community, society) and over an adequate period of time.
A program called Total Community Mobilization sent 450 AIDS counselors door-to-door, giving prevention advice, urging HIV testing and referring infected people to treatment.
[38]In Nigeria, There was a somewhat different result in a study of young Nigerians, ages 15 to 24, most unmarried, living in the city and working in semiskilled jobs.
The TeachAids prevention software, developed at Stanford University, was distributed to every primary, secondary, and tertiary educational institution in the country, reaching all learners from 6 to 24 years of age nationwide.
The initiative was formed to "accelerate efforts by Heads of State and Government to implement their commitments for the fight against HIV/AIDS, and to mobilize the required national and international resources.
[28] This Roadmap outlines a set of African-developed strategies to strengthen shared responsibility and international cooperation for achieving sustainable AIDS solutions in Africa by 2015.
[45] The Joint United Nations Program on HIV/AIDS reported that the following sixteen African nations in 2012 "ensure[d] that more than three-quarters of pregnant women living with HIV receive antiretroviral medicine to prevent transmission to their child": Botswana, Gabon, Gambia, Ghana, Mauritius, Mozambique, Namibia, Rwanda, São Tomé and Principe, Seychelles, Sierra Leone, South Africa, Eswatini, Tanzania, Zambia and Zimbabwe.
[48] In addition, in sub-Saharan Africa AIDS is the leading killer and a large reason for the high transmission rates is because of the lack of education provided to youth.
For African countries with advanced medical facilities, patents on many drugs have hindered the ability to make low cost alternatives.
[51] Natural disasters and conflict are also major challenges, as the resulting economic problems people face can drive many young women and girls into patterns of sex work in order to ensure their livelihood or that of their family, or else to obtain safe passage, food, shelter or other resources.
[70] Pressure from both Christian and Muslim religious leaders has resulted in the banning of a number of safe-sex campaigns, including condom promoting advertisements.
[citation needed] Health units that conduct sero surveys rarely operate in remote rural communities, and the data collected also does not measure people who seek alternate healthcare.
[citation needed] A minority of scientists claim that as many as 40 percent of HIV infections in African adults may be caused by unsafe medical practices rather than by sexual activity.
[75] The World Health Organization states that about 2.5 percent of HIV infections in Sub-Saharan Africa are caused by unsafe medical injection practices and the "overwhelming majority" by unprotected sex.
The latter includes practices such as multiple sexual partners and unprotected sex, high-risk cultural patterns that have been implicated in the much greater spread of HIV in the subcontinent.
The director of the Centre for Disease Control – Uganda, Wuhib Tadesse, said in 2011 that, for every person started on antiretroviral therapy, there are three new HIV infections[,] and this is unsustainable.
[77] Of the nine southern African countries (Botswana, Lesotho, Malawi, Mozambique, Namibia, South Africa, Eswatini, Zambia, and Zimbabwe), four are estimated to have an infection rate of over 15 percent.
[98] Based on 2011 data, Eswatini's crude death rate of 19.51 per 1,000 people per year was the third highest in the world, behind only Lesotho and Sierra Leone.
[102] "Tuberculosis and HIV co-infections are associated with special diagnostic and therapeutic challenges and constitute an immense burden on healthcare systems of heavily infected countries like Ethiopia.
[105] In the following 20 African countries, the cases-per-100,000 coinfection rate has increased at least 20 percent between 2000 and 2011: Algeria, Angola, Chad, Comoros, Republic of the Congo, Democratic Republic of the Congo, Equatorial Guinea, The Gambia, Lesotho, Liberia, Mauritania, Mauritius, Morocco, Mozambique, Senegal, Sierra Leone, South Africa, Eswatini, Togo, and Tunisia.