Cluster headache
[2] Attacks often occur in clusters which typically last for weeks or months and occasionally more than a year.
[2][4] Measures recommended to decrease the frequency of attacks include steroid injections, galcanezumab, civamide, verapamil, or oral glucocorticoids such as prednisone.
The pain is typically greater than in other headache conditions, including migraines, and is usually described as burning, stabbing, drilling or squeezing.
[18][19] Dr. Peter Goadsby, Professor of Clinical Neurology at University College London, a leading researcher on the condition has commented: "Cluster headache is probably the worst pain that humans experience.
I know that's quite a strong remark to make, but if you ask a cluster headache patient if they've had a worse experience, they'll universally say they haven't.
So you can imagine that these people give birth without anesthetic once or twice a day, for six, eight, or ten weeks at a time, and then have a break.
[2][21] Cluster headache attack is accompanied by at least one of the following autonomic symptoms: drooping eyelid, pupil constriction, redness of the conjunctiva, tearing, runny nose and less commonly, facial blushing, swelling, or sweating, typically appearing on the same side of the head as the pain.
[21] Similar to a migraine, sensitivity to light (photophobia) or noise (phonophobia) may occur during a cluster headache.
Secondary effects may include the inability to organize thoughts and plans, physical exhaustion, confusion, agitation, aggressiveness, depression, and anxiety.
The recurrence of headache cluster grouping may occur more often around solstices, or seasonal changes, sometimes showing circannual periodicity.
If headache attacks occur for more than a year without pain-free remission of at least three months, the condition is classified as chronic.
The frequency, severity, and duration of headache attacks experienced by people during these cycles varies between individuals and does not demonstrate complete remission of the episodic form.
This is supported by a relatively high success ratio of deep-brain stimulation therapy on the posterior hypothalamic grey matter.
[31][32] People with a first degree relative with the condition are about 14–48 times more likely to develop it themselves,[1] and around 8 to 10% of persons with cluster headaches have a family history.
[1] People with cluster headaches may be predisposed to certain traits, including smoking or other lifestyle habits.
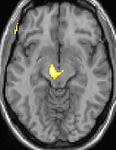
[35] Positron emission tomography (PET) scans indicate the brain areas which are activated during attack only, compared to pain free periods.
[21] A detailed oral history aids practitioners in correct differential diagnosis, as there are no confirmatory tests for cluster headache.
[16] Individuals with cluster headaches typically experience diagnostic delay before correct diagnosis.
[39] People are often misdiagnosed due to reported neck, tooth, jaw, and sinus symptoms and may unnecessarily endure many years of referral to ear, nose and throat (ENT) specialists for investigation of sinuses; dentists for tooth assessment; chiropractors and manipulative therapists for treatment; or psychiatrists, psychologists, and other medical disciplines before their headaches are correctly diagnosed.
[40] Under-recognition of cluster headaches by health care professionals is reflected in consistent findings in Europe and the United States that the average time to diagnosis is around seven years.
[48] Preventive treatments are used to reduce or eliminate cluster headache attacks; they are generally used in combination with abortive and transitional techniques.
[50] Preventive therapy with verapamil is believed to work because it has an effect on the circadian rhythm and on CGRPs as CGRP-release is controlled by voltage-gated calcium channels.
[56] There are two primary treatments for acute CH: oxygen and triptans,[2] but they are underused due to misdiagnosis of the syndrome.
[64] Prescription of opioid medication may additionally lead to further delay in differential diagnosis, undertreatment, and mismanagement.
[11] Octreotide administered subcutaneously has been demonstrated to be more effective than placebo for the treatment of acute attacks.
[67] The first complete description of cluster headache was given by the London neurologist Wilfred Harris in 1926, who named the disease migrainous neuralgia.
[73] Robert Shapiro, a professor of neurology, says that while cluster headaches are about as common as multiple sclerosis with a similar disability level, as of 2013, the US National Institutes of Health had spent $1.872 billion on research into multiple sclerosis in one decade, but less than $2 million on cluster headache research in 25 years.
[74] Some case reports suggest that ingesting tryptamines such as LSD, psilocybin (as found in hallucinogenic mushrooms), or DMT can abort attacks and interrupt cluster headache cycles.
[75][76] The hallucinogen DMT has a chemical structure that is similar to the triptan sumatriptan, indicating a possible shared mechanism in preventing or stopping migraine and TACs.
[77][78][79] Fremanezumab, a humanized monoclonal antibody directed against calcitonin gene-related peptides alpha and beta, was in phase 3 clinical trials for cluster headaches, but the studies were stopped early due to a futility analysis demonstrating that a successful outcome was unlikely.