Black lung disease
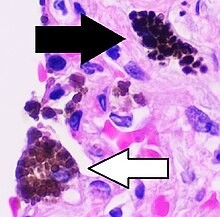
[3] Inhaled coal dust progressively builds up in the lungs and leads to inflammation, fibrosis, and in worse cases, necrosis.
[10] In the US, a 2018 study by the National Institute of Occupational Safety and Health shows a resurgence among veteran coalminers, recording the highest rate of BLD in roughly two decades.
Coal dust provides a sufficient stimulus for the macrophage to release various products, including enzymes, cytokines, oxygen radicals, and fibroblast growth factors,[13] which are important in the development of inflammation and fibrosis in BLD.
Simple BLD is marked by the presence of 1–2 mm (0.039–0.079 in) nodular aggregations of anthracotic macrophages, supported by a fine collagen network, within the lungs.
These structures occur most frequently around the initial site of coal dust accumulation—the upper regions of the lungs around respiratory bronchioles.
[16] Continued exposure to coal dust following the development of simple BLD may progress to complicated BLD with progressive massive fibrosis (PMF), wherein large masses of dense fibrosis develop, usually in the upper lung zones, measuring greater than 1 cm (0.39 in) in diameter, with accompanying decreased lung function.
[18] Pneumoconiosis can also be caused by inhaling other dusts including aluminum, antimony, barium, graphite, iron, kaolin, mica, and talc.
After the death of Lewis, the union dropped its opposition to calling black lung a disease and realized the financial advantages of a fund for its disabled members.
In the Federal Coal Mine Health and Safety Act of 1969, the US Congress set up standards to reduce dust and created the Black Lung Disability Trust.
Equally important was a "rate retention" clause that allowed workers with progressive lung disease to transfer to jobs with lower exposure without loss of pay, seniority, or benefits.
[24] After the Federal Coal Mine Health and Safety Act of 1969 became law in the United States, the percentage of American miners with black lung disease decreased by about 90 percent.
[29] A 2016–17 investigation by National Public Radio found that NIOSH had under-reported cases of PMF (a complication of black lung) by at least a factor of 20.
[32] New U.S. MSHA rules took effect in August 2016 that lowered maximum allowed dust concentrations for surface and underground mines, and exposure by miners who have been found to be developing pneumoconiosis.
[33] Work to investigate the relationship between respirable dust exposure and coal worker's pneumoconiosis was carried out in the United Kingdom by the Institute of Occupational Medicine.
The point of their research was to answer some key questions that would shed some light on the prevalence and danger of black lung disease in specific subpopulations.
The report's first finding was the rate of black lung disease across the United States, with an average of 4.34 cases and 3.44 deaths per county.
[34] The numbers collected may even be undercounted as the Coal Workers Health Surveillance Programs had a low output of screenings, and compensation approval rates were very slow.
A third finding of the study compared rates of black lung disease in the Navajo nation to the residents of Appalachia and the rest of the country.
The last finding of the study was to determine the correlation of residential coal burning and instances of black lung disease.
[34] Residential coal burning may be a contributing factor and not the main cause though, as these areas also have more mines and miners that could develop the disease from their occupation.