Crohn's disease
[3][13][14][15] It results in a chronic inflammatory disorder, in which the body's immune system defends the gastrointestinal tract, possibly targeting microbial antigens.
[1] In those newly diagnosed, a corticosteroid may be used for a brief period of time to improve symptoms rapidly, alongside another medication such as either methotrexate or a thiopurine to prevent recurrence.
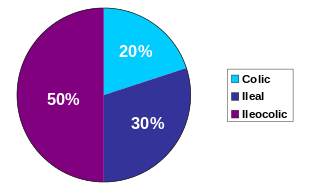
[3] The disease was named after gastroenterologist Burrill Bernard Crohn, who in 1932, together with Leon Ginzburg (1898–1988) and Gordon D. Oppenheimer (1900–1974) at Mount Sinai Hospital in New York, described a series of patients with inflammation of the terminal ileum of the small intestine, the area most commonly affected by the illness.
[51] Inflammation may also involve the white part of the eye (sclera) or the overlying connective tissue (episclera), which causes conditions called scleritis and episcleritis, respectively.
The sudden onset of severe abdominal, back, or flank pain in patients with IBD, particularly if different from the usual discomfort, should lead to inclusion of a renal stone in the differential diagnosis.
[56] Urological manifestations in patients with IBD may include ureteral calculi, enterovesical fistula, perivesical infection, perinephric abscess, and obstructive uropathy with hydronephrosis.
Ureteral compression is associated with retroperitoneal extension of the phlegmonous inflammatory process involving the terminal ileum and cecum, and may result in hydronephrosis severe enough to cause hypertension.
The clinical presentation may include chest pain, dyspnea, or in severe cases pericardial tamponade requiring rapid drainage.
[56] Crohn's disease also increases the risk of blood clots;[55] painful swelling of the lower legs can be a sign of deep venous thrombosis, while difficulty breathing may be a result of pulmonary embolism.
Erythema nodosum is the most common type of skin problem, occurring in around 8% of people with Crohn's disease, producing raised, tender red nodules usually appearing on the shins.
[70][71] Other very rare dermatological manifestations include: pyostomatitis vegetans, erythema multiforme, epidermolysis bullosa acquista (described in a case report), and metastatic CD (the spread of Crohn's inflammation to the skin[47]).
Persistent vomiting and nausea may indicate stenosis from small bowel obstruction or disease involving the stomach, pylorus, or duodenum.
[90] Major complications of Crohn's disease include bowel obstruction, abscesses, free perforation, and hemorrhage, which in rare cases may be fatal.
Such individuals may require oral supplements to increase their caloric intake, or in severe cases, total parenteral nutrition (TPN).
[98] A substantial body of data has emerged in recent years to suggest that the primary defect in Crohn's disease is actually one of relative immunodeficiency.
The suggestion therefore is that Crohn's pathogenesis actually results from partial immunodeficiency, a theory that coincides with the frequent recognition of a virtually identical, non-infectious inflammatory bowel disease arising in patients with congenital monogenic disorders impairing phagocyte function.
This same gene may reduce innate and adaptive immunity in gastrointestinal tissue and impair the ability to resist infection by the MAP bacterium.
[143] Mouse studies have suggested some symptoms of Crohn's disease, ulcerative colitis, and irritable bowel syndrome have the same underlying cause.
[6] The introduction of hormonal contraception in the United States in the 1960s is associated with a dramatic increase in incidence, and one hypothesis is that these drugs work on the digestive system in ways similar to smoking.
Biopsies may also show chronic mucosal damage, as evidenced by blunting of the intestinal villi, atypical branching of the crypts, and a change in the tissue type (metaplasia).
[180] MRI techniques such as diffusion-weighted imaging and high-resolution imaging are more sensitive in detecting ulceration and inflammation compared to CT.[181][182] A complete blood count may reveal anemia, which commonly is caused by blood loss leading to iron deficiency or by vitamin B12 deficiency, usually caused by ileal disease impairing vitamin B12 absorption.
[184] Other causes of anemia include medication used in treatment of inflammatory bowel disease, like azathioprine, which can lead to cytopenia, and sulfasalazine, which can also result in folate deficiency.
Certain lifestyle changes can reduce symptoms, including dietary adjustments, elemental diet, proper hydration, and smoking cessation.
[209] Fatigue can be helped with regular exercise, a healthy diet, and enough sleep, and for those with malabsorption of vitamin B12 due to disease or surgical resection of the terminal ileum, cobalamin injections.
[36] The monoclonal antibody ustekinumab appears to be a safe treatment option, and may help people with moderate to severe active Crohn's disease.
[218] The gradual loss of blood from the gastrointestinal tract, as well as chronic inflammation, often leads to anemia, and professional guidelines suggest routinely monitoring for this.
After a resection, scar tissue builds up, which can cause strictures, which form when the intestines become too small to allow excrement to pass through easily, which can lead to a blockage.
[234] The use of oral probiotic supplements to modify the composition and behaviour of the gastrointestinal microbiome has been researched to understand whether it may help to improve remission rate in people with Crohn's disease.
However, only two controlled trials were available in 2020, with no clear overall evidence of higher remission nor lower adverse effects, in people with Crohn's disease receiving probiotic supplementation.
Later that year, he, along with colleagues Leon Ginzburg and Gordon Oppenheimer, published the case series "Regional ileitis: a pathologic and clinical entity".