Congenital disorder of glycosylation
Common manifestations include ataxia; seizures; retinopathy; liver disease; coagulopathies; failure to thrive (FTT); dysmorphic features (e.g., inverted nipples and subcutaneous fat pads); pericardial effusion, skeletal abnormalities, and hypotonia.
[4] Ocular abnormalities of PMM2-CDG include: myopia, infantile esotropia, delayed visual maturation, peripheral neuropathy (PN), strabismus, nystagmus, optic disc pallor, and reduced rod function on electroretinography.
Lack thereof leads to leukocytosis and increased sensitivity to infections as seen in SLC35C1-CDG(CDG-IIc); caused by a GDP-fucose (Fuc) transporter deficiency.
The mature LLO is transferred co-translationally to consensus sequence Asn residues in the nascent protein, and is further modified by trimming and re-building in the Golgi.
[30] Historically, CDGs are classified as Types I and II (CDG-I and CDG-II), depending on the nature and location of the biochemical defect in the metabolic pathway relative to the action of oligosaccharyltransferase.
[33] The reason for the new nomenclature was the fact that proteins not directly involved in glycan synthesis (such as members of the COG-family[34] and vesicular H+-ATPase)[35] were found to be causing the glycosylation defect in some CDG patients.
[42] The first CDG patients (twin sisters) were described in 1980 by Jaeken et al.[43] Their main features were psychomotor retardation, cerebral and cerebellar atrophy and fluctuating hormone levels (e.g.prolactin, FSH and GH).
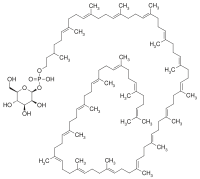
This enzyme is responsible for the interconversion of mannose-6-phosphate and mannose-1-phosphate, and its deficiency leads to a shortage in GDP-mannose and dolichol (Dol)-mannose (Man), two donors required for the synthesis of the lipid-linked oligosaccharide precursor of N-linked glycosylation.
[45] In 1998, Niehues described a new CDG syndrome, MPI-CDG, which is caused by mutations in the enzyme metabolically upstream of PMM2, phosphomannose isomerase (PMI).