Defibrillation
[4] Although the person may still be critically ill, cardioversion normally aims to end poorly perfusing cardiac arrhythmias, such as supraventricular tachycardia.
A healthcare provider first diagnoses the cardiac rhythm and then manually determine the voltage and timing for the electrical shock.
For instance, every NHS ambulance in the United Kingdom is equipped with a manual defibrillator for use by the attending paramedics and technicians.
[19] As early defibrillation can significantly improve VF outcomes, AEDs have become publicly available in many easily accessible areas.
They constantly monitor the patient's heart rhythm, and automatically administer shocks for various life-threatening arrhythmias, according to the device's programming.
This is considered a medical emergency, as it depletes the device's battery life, causes significant discomfort and anxiety to the patient, and in some cases may actually trigger life-threatening arrhythmias.
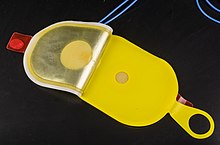
[22] The connection between the defibrillator and the patient consists of a pair of electrodes, each provided with electrically conductive gel in order to ensure a good connection and to minimize electrical resistance, also called chest impedance (despite the DC discharge) which would burn the patient.
However, the use of solid-gel presents a higher risk of burns during defibrillation, since wet-gel electrodes more evenly conduct electricity into the body.
The most well-known type of electrode (widely depicted in films and television) is the traditional metal "hard" paddle with an insulated (usually plastic) handle.
Many hospitals in the United States continue the use of paddles, with disposable gel pads attached in most cases, due to the inherent speed with which these electrodes can be placed and used.
If defibrillation is required, the machine is charged, and the shock is delivered, without any need to apply any additional gel or to retrieve and place any paddles.
They may be used for multiple shocks in a single course of treatment, but are replaced if (or in case) the patient recovers then reenters cardiac arrest.
Researchers have created a software modeling system capable of mapping an individual's chest and determining the best position for an external or internal cardiac defibrillator.
[25][26] Cardiac cells require a strong electrical stimulus to raise their transmembrane potential to the activation threshold.
[25][26] Only a small amount of electrical current enters the cell due to high membrane impedance.
[25][26] Irregular rhythms often result from re-entrant circuits, where electrical impulses circle within the heart tissue due to areas of slow conduction or unidirectional block.
They discovered that small electrical shocks could induce ventricular fibrillation in dogs, and that larger charges would reverse the condition.
This invention was called the Hyman Otor where a hollow needle is used to pass an insulated wire to the heart area to deliver the electrical shock.
Kouwenhoven studied the relationship between electric shocks and their effects on the human heart when he was a student at Johns Hopkins University School of Engineering.
Beck used internal paddles on either side of the heart, along with procainamide, an antiarrhythmic drug, and achieved return of a perfusing cardiac rhythm.
The technique was often ineffective in reverting VF while morphological studies showed damage to the cells of the heart muscle post-mortem.
[40] Humphrey immediately recognized importance of reanimation research and after that a number of American doctors visited Gurvich.
At the same time, Humphrey worked on establishing a federal program in the National Institute of Health in physiology and medicine, telling Congress: "Let's compete with U.S.S.R. in research on reversibility of death".
The studies showed that the biphasic truncated waveform could be more efficacious while requiring the delivery of lower levels of energy to produce defibrillation.
This was pioneered at Sinai Hospital in Baltimore by a team that included Stephen Heilman, Alois Langer, Jack Lattuca, Morton Mower, Michel Mirowski, and Mir Imran, with the help of industrial collaborator Intec Systems of Pittsburgh.
[45] In 1972, Lown stated in the journal Circulation – "The very rare patient who has frequent bouts of ventricular fibrillation is best treated in a coronary care unit and is better served by an effective antiarrhythmic program or surgical correction of inadequate coronary blood flow or ventricular malfunction.
In fact, the implanted defibrillator system represents an imperfect solution in search of a plausible and practical application.
Despite the lack of financial backing and grants, they persisted and the first device was implanted in February 1980 at Johns Hopkins Hospital by Dr. Levi Watkins Jr. assisted by Vivien Thomas.
As devices that can quickly produce dramatic improvements in patient health, defibrillators are often depicted in movies, television, video games and other fictional media.
After recovering, Kerry Packer donated a large sum to the Ambulance Service of New South Wales in order that all ambulances in New South Wales should be fitted with a personal defibrillator, which is why defibrillators in Australia are sometimes colloquially called "Packer Whackers".