In vitro fertilisation
According to UK's National Institute for Health and Care Excellence (NICE) guidelines, IVF treatment is appropriate in cases of unexplained infertility for people who have not conceived after 2 years of regular unprotected sexual intercourse.
[18] According to the 2021 National Summary Report compiled by the Society for Assisted Reproductive Technology (SART), the mean number of embryos transfers for patients achieving live birth go as follows:[19] Effective from 15 February 2021 the majority of Australian IVF clinics publish their individual success rate online via YourIVFSuccess.com.au.
The 2019 summary compiled by the SART the following data for non-donor eggs (first embryo transfer) in the United States:[21] In 2006, Canadian clinics reported an average pregnancy rate of 35%.
[23] The main potential factors that influence pregnancy (and live birth) rates in IVF have been suggested to be maternal age, duration of infertility or subfertility, bFSH and number of oocytes, all reflecting ovarian function.
[40] The review found that oral antioxidants given to the sperm donor with male factor or unexplained subfertility may improve live birth rates, but more evidence is needed.
[48] Mild IVF[49] is a method where a small dose of ovarian stimulating drugs are used for a short duration during a natural menstrual cycle aimed at producing 2–7 eggs and creating healthy embryos.
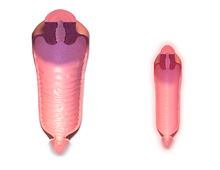
[51] When the ovarian follicles have reached a certain degree of development, induction of final oocyte maturation is performed, generally by an injection of human chorionic gonadotropin (hCG).
This Deep Learning software substitutes manual classifications with a ranking system based on an individual embryo's predicted genetic status in a non-invasive fashion.
A Cochrane review found that hCG or progesterone given during the luteal phase may be associated with higher rates of live birth or ongoing pregnancy, but that the evidence is not conclusive.
However, a systematic review and meta-analysis of existing randomised controlled trials came to the result that there is no evidence of a beneficial effect of PGS with cleavage-stage biopsy as measured by live birth rate.
[70] Still, as an expansion of IVF, patients who can benefit from PGS/PGD include: PGS screens for numeral chromosomal abnormalities while PGD diagnosis the specific molecular defect of the inherited disease.
Multiple births are related to increased risk of pregnancy loss, obstetrical complications, prematurity, and neonatal morbidity with the potential for long term damage.
Strict limits on the number of embryos that may be transferred have been enacted in some countries (e.g. Britain, Belgium) to reduce the risk of high-order multiples (triplets or more), but are not universally followed or accepted.
"[96] The authors of the Danish national registry study speculate: "our results suggest that the reported increased prevalence of congenital malformations seen in singletons born after assisted reproductive technology is partly due to the underlying infertility or its determinants.
[105] In some cases, laboratory mix-ups (misidentified gametes, transfer of wrong embryos) have occurred, leading to legal action against the IVF provider and complex paternity suits.
[109] Pre-implantation genetic diagnosis (PGD) is criticised for giving select demographic groups disproportionate access to a means of creating a child possessing characteristics that they consider "ideal".
State officials allege that performing Suleman's procedure is evidence of unreasonable judgment, substandard care, and a lack of concern for the eight children she would conceive and the six she was already struggling to raise.
For a baby conceived naturally, the father's identity is determined by a legal presumption (chazakah) of legitimacy: rov bi'ot achar ha'baal – a woman's sexual relations are assumed to be with her husband.
[157]: 336 In certain countries, including Austria, Italy, Estonia, Hungary, Spain and Israel, the male does not have the full ability to withdraw consent to storage or use of embryos once they are fertilised.
For gay male couples, many elect to use IVF through gestational surrogacy, where one partner's sperm is used to fertilise a donor ovum, and the resulting embryo is transplanted into a surrogate carrier's womb.
Literature shows that transgender men report uncomfortable procedures and interactions during their pregnancies as well as feeling misgendered due to gendered terminology used by healthcare providers.
[176] All patients experienced menses and normal AMH, FSH and E2 levels and antral follicle counts after coming off testosterone, which allowed for successful oocyte retrieval.
Biological reproductive options available to transgender women include, but are not limited to, IVF and IUI with the trans woman's sperm and a donor or a partner's eggs and uterus.
[citation needed] The Human Fertilisation and Embryology Authority said in September 2018 that parents who are limited to one cycle of IVF, or have to fund it themselves, are more likely choose to implant multiple embryos in the hope it increases the chances of pregnancy.
The president of the Royal College of Obstetricians and Gynaecologists said that funding 3 cycles was "the most important factor in maintaining low rates of multiple pregnancies and reduce(s) associated complications".
Eleven states require coverage for both fertility preservation and IVF: Colorado, Connecticut, Delaware, Maryland, Maine, New Hampshire, New Jersey, New York, Rhode Island, Utah, and Washington D.C.[206] The states that have infertility coverage laws are Arkansas, California, Colorado, Connecticut, Delaware, Hawaii, Illinois, Louisiana, Maryland, Massachusetts, Montana, New Hampshire, New Jersey, New York, Ohio, Rhode Island, Texas, Utah, and West Virginia.
[216][217] In spite of Costa Rican government and strong religious opposition, the IVF ban has been struck down by the Inter-American Court of Human Rights in a decision of 20 December 2012.
[220] All major restrictions on single but infertile people using IVF were lifted in Australia in 2002 after a final appeal to the Australian High Court was rejected on procedural grounds in the Leesa Meldrum case.
[221] Victoria's government announced changes to its IVF law in 2007 eliminating remaining restrictions on fertile single women and lesbians, leaving South Australia as the only state maintaining them.
Frozen embryos at an IVF clinic were accidentally destroyed resulting in a lawsuit during which the attorneys for the plaintiff sought damages under the Wrongful Death of a Minor Act.