Endometrial cancer
[2][10] Abnormal menstrual cycles or extremely long, heavy, or frequent episodes of bleeding in women before menopause may also be a sign of endometrial cancer.
[20] Polycystic ovary syndrome (PCOS), which also causes irregular or no ovulation, is associated with higher rates of endometrial cancer for the same reasons as obesity.
[23] Unopposed estrogen raises an individual's risk of endometrial cancer by 2–10 fold, depending on weight and length of therapy.
[18] Carcinogenesis in Lynch syndrome comes from a mutation in MLH1 or MLH2: genes that participate in the process of mismatch repair, which allows a cell to correct mistakes in the DNA.
[18] Common genetic variation has also been found to affect endometrial cancer risk in large-scale genome-wide association studies.
[28][29] Sixteen genomic regions have been associated with endometrial cancer and the common variants explain up to 7% of the familial relative risk.
[31] Mendelian randomization analyses have established potential protective factors such as LDL cholesterol, later age of menarche and sex hormone binding globulin.
CTNNB1 (beta-catenin; a transcription gene) mutations are found in 14–44% of endometrial cancers and may indicate a good prognosis, but the data is unclear.
A study from 2024 indicates that transvaginal ultrasound provides diagnostic performance comparable to magnetic resonance imaging regarding the myometrial infiltration assessment.
Some women with Lynch syndrome elect to have a prophylactic hysterectomy and salpingo-oophorectomy to greatly reduce the risk of endometrial and ovarian cancer.
CT scans are used for preoperative imaging of tumors that appear advanced on physical exam or have a high-risk subtype (at high risk of metastasis).
Type I endometrial cancers are often low-grade, minimally invasive into the underlying uterine wall (myometrium), estrogen-dependent, and have a good outcome with treatment.
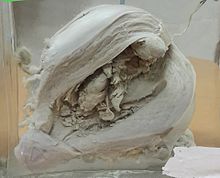
[15] In endometrioid adenocarcinoma, the cancer cells grow in patterns reminiscent of normal endometrium, with many new glands formed from columnar epithelium with some abnormal nuclei.
The most common finding is a well-differentiated endometrioid adenocarcinoma,[50] which is composed of numerous, small, crowded glands with varying degrees of nuclear atypia, mitotic activity, and stratification.
Frank adenocarcinoma may be distinguished from atypical hyperplasia by the finding of clear stromal invasion, or "back-to-back" glands which represent nondestructive replacement of the endometrial stroma by the cancer.
[64][65] The 2009 FIGO staging system is as follows:[66][67] Myometrial invasion and involvement of the pelvic and para-aortic lymph nodes are the most commonly seen patterns of spread.
[23] Surgical treatment typically consists of hysterectomy including a bilateral salpingo-oophorectomy, which is the removal of the uterus, and both ovaries and Fallopian tubes.
[71] The few contraindications to surgery include inoperable tumor, massive obesity, a particularly high-risk operation, or a desire to preserve fertility.
[16] Adjuvant chemotherapy is a recent innovation, consisting of some combination of paclitaxel (or other taxanes like docetaxel), doxorubicin (and other anthracyclines), and platins (particularly cisplatin and carboplatin).
It can be delivered through vaginal brachytherapy (VBT), which is becoming the preferred route due to its reduced toxicity, or external beam radiotherapy (EBRT).
Also, endometrial stromal sarcomas can be treated with hormonal agents, including tamoxifen, hydroxyprogesterone caproate, letrozole, megestrol acetate, and medroxyprogesterone.
[32][44][82] Periodic MRIs or CT scans may be recommended in advanced disease and women with a history of endometrial cancer should receive more frequent pelvic examinations for the five years following treatment.
[89] Following diagnosis, quality of life is also positively associated with a healthy lifestyle (no obesity, high-quality diet, physical activity).
[37] Cancers can be analyzed using genetic techniques (including DNA sequencing and immunohistochemistry) to determine if certain therapies specific to mutated genes can be used to treat it.
[95] Bevacizumab and tyrosine kinase inhibitors, which inhibit angiogenesis, are being researched as potential treatments for endometrial cancers with high levels of vascular endothelial growth factor.
Preliminary research has shown that the levonorgestrel IUD placed for a year, combined with six monthly injections of gonadotropin-releasing hormone, can stop or reverse the progress of endometrial cancer in young women; specifically complex atypical hyperplasia however the results have been inconclusive.
[98][99] In surgery, research has shown that complete pelvic lymphadenectomy along with hysterectomy in stage 1 endometrial cancer does not improve survival and increases the risk of negative side effects, including lymphedema.
Other research is exploring the potential of identifying the sentinel lymph nodes for biopsy by injecting the tumor with dye that shines under infrared light.
Intensity modulated radiation therapy is currently under investigation, and already used in some centers, for application in endometrial cancer, to reduce side effects from traditional radiotherapy.
[95] There is not enough evidence to determine if people with endometrial cancer benefit from additional behavioural and life style interventions that are aimed at losing excess weight.








- Left panel shows H&E staining and low magnification, where presence of small metastases is hard to see.
- Middle panel shows immunohistochemistry for CK AE1/AE3 , which highlights even small tumor nests.
- The right panel shows high magnification on a positive area, confirming adenocarcinoma, as it shows tumor cells with large nuclei and prominent nucleoli.

