Babesiosis
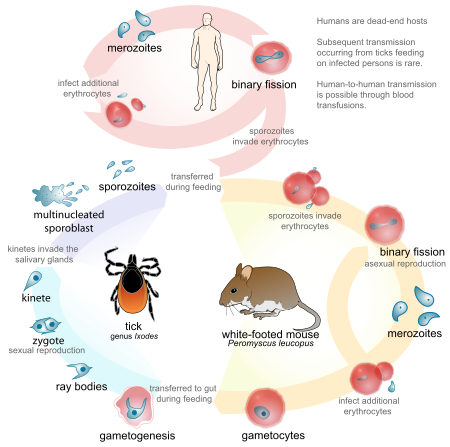
[2] Human babesiosis transmission via tick bite is most common in the Northeastern and Midwestern United States and parts of Europe, and sporadic throughout the rest of the world.
[9] A reported increase in human babesiosis diagnoses in the 2000s is thought to be caused by more widespread testing and higher numbers of people with immunodeficiencies coming in contact with ticks, the disease vector.
The main species in each clade are:[citation needed] Babesia parasites reproduce in red blood cells, where they can be seen as cross-shaped inclusions (four merozoites asexually budding, but attached forming a structure looking like a "Maltese cross")[11] and cause hemolytic anemia, quite similar to malaria.
Unlike the Plasmodium parasites that cause malaria, Babesia species rarely exhibit an exoerythrocytic phase with trophozoite forms.
[citation needed] In bovine species, the organism causes hemolytic anemia, so an infected animal shows pale mucous membranes initially.
It develops in patients who live in or travel to an endemic area or receive a contaminated blood transfusion within the preceding 9 weeks, so this aspect of the medical history is vital.
[13] So-called "Maltese cross formations" on the blood film are diagnostic (pathognomonic) of babesiosis since they are not seen in malaria, the primary differential diagnosis.
[11] Careful examination of multiple smears may be necessary, since Babesia may infect less than 1% of circulating red blood cells, thus be easily overlooked.
[14] Serologic testing for antibodies against Babesia (both IgG and IgM) can detect low-level infection in cases with high clinical suspicion, but negative blood film examinations.
Since detectable antibody responses require about a week after infection to develop, serologic testing may be falsely negative early in the disease course.
Diagnosis is confirmed by observation of merozoites on a thin film blood smear examined at maximum magnification under oil using Romonovski stains (methylene blue and eosin).
[citation needed] Cerebral babesiosis is suspected in vivo when neurological signs (often severe) are seen in cattle that are positive for B. bovis on blood smear, but this has yet to be proven scientifically.
Diagnosis is confirmed post-mortem by observation of Babesia-infected erythrocytes sludged in the cerebral cortical capillaries in a brain smear.
[21] Extracts of the poisonous, bulbous plant Boophone disticha are used in the folk medicine of South Africa to treat equine babesiosis.
decoloratus transmit several species of Babesia to livestock, causing considerable economic losses to farmers in tropical and subtropical regions.
[citation needed] In the United States, the majority of babesiosis cases are caused by B. microti, and occur in the Northeast and northern Midwest from May through October.
[25][26][27][28][29] The Centers for Disease Control and Prevention now requires state health departments to report infections using Form OMB No.
[38] In 1888, Victor Babeș identified the microorganisms in red blood cells as the cause of febrile hemoglobinuria in cattle.
[citation needed] Equine babesiosis (caused by the protozoan Theileria equi) is also known as piroplasmosis (from the Latin piro, meaning pear + Greek plasma, a thing formed).
B. imitans causes a mild form of the disease that frequently resolves without treatment (dogs in Southeast Asia).