Esketamine
[16][10] Esketamine is not used by infusion into a vein for depression as it is only FDA-approved in the form of a nasal spray under direct medical supervision for this indication (the parent compound ketamine is most often administered intravenously).
[10][5] Adverse effects of esketamine include dissociation, dizziness, sedation, nausea, vomiting, vertigo, numbness, anxiety, lethargy, increased blood pressure, and feelings of drunkenness.
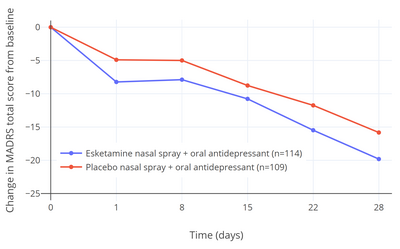
[22][24][16][23] In the one positive short-term efficacy study (TRANSFORM-2), there was a 4.0-point difference between esketamine and placebo on the Montgomery–Åsberg Depression Rating Scale (MADRS) after 4 weeks of treatment (P = 0.020).
[22][10][25] In the two negative short-term efficacy trials that did not reach statistical significance (TRANSFORM-1 and -3), the differences in MADRS reductions between esketamine and placebo were –3.2 (P = 0.088) and –3.6 (P = 0.059) after 4 weeks of treatment.
[23] The 4.0-point additional reduction in MADRS score with esketamine over placebo in the single positive efficacy trial corresponds to less than "minimal improvement" and has been criticized as being below the threshold for clinically meaningful change.
[22][24] A difference of at least 6.5 points was originally suggested by the trial investigators to be a reasonable threshold for clinical significance.
[10] The secondary efficacy measure in the trials was change in Clinical Global Impression of Suicidal Severity - Revised (CGI-SS-r) 24 hours after the first dose of esketamine.
[10][15] Expectations were initially very high for ketamine and esketamine for treatment of depression based on early small-scale clinical studies, with discovery of the rapid and ostensibly robust antidepressant effects of ketamine described by some authors as "the most important advance in the field of psychiatry in the past half century".
[39] However, these meta-analyses have involved largely non-directly comparative studies with dissimilar research designs and patient populations.
[40][15][41] However, the study was small and underpowered, and more research is still needed to better-characterize the comparative antidepressant effects of ketamine and esketamine.
[42][43] In February 2019, an outside panel of experts recommended in a 14–2 vote that the FDA approve the nasal spray version of esketamine for treatment-resistant depression, provided that it be given in a clinical setting, with people remaining on site for at least two hours after.
[44][45] The reasoning for this requirement is that trial participants temporarily experienced sedation, visual disturbances, trouble speaking, confusion, numbness, and feelings of dizziness during immediately after.
[46] The approval of esketamine for treatment-resistant depression by the FDA was controversial due to limited and mixed evidence of efficacy and safety.
[48] The Institute for Clinical and Economic Review (ICER), which evaluates cost effectiveness of drugs analogously to the National Institute for Health and Care Excellence (NICE) in the United Kingdom, declined to recommend esketamine for depression due to its steep cost and modest efficacy, deeming it not sufficiently cost-effective.
[25][50] Other agents, like the atypical antipsychotics aripiprazole (Abilify) and quetiapine (Seroquel), have been approved for use in the adjunctive therapy of major depressive disorder in people with a partial response to treatment.
[25] In a meta-analysis conducted internally by the FDA during its evaluation of esketamine for treatment-resistant depression, the FDA reported a standardized mean difference (SMD) of esketamine for treatment-resistant depression of 0.28 using the three phase III short-term efficacy trials conducted by Janssen.
[25] The most common adverse effects of esketamine for depression (≥5% incidence) include dissociation, dizziness, sedation, nausea, vomiting, vertigo, numbness, anxiety, lethargy, increased blood pressure, and feelings of drunkenness.
This difference may be responsible for the fact that esketamine generally has a more dissociative or hallucinogenic effect while arketamine is reportedly more relaxing.
[5][20] In addition to its anesthetic effects, the medication showed properties of being a rapid-acting antidepressant, and was subsequently investigated for use as such.
[19] In August 2020, it was approved by the U.S. Food and Drug Administration (FDA) with the added indication for the short-term treatment of suicidal thoughts.