Fatal insomnia
Fatal insomnia is an extremely rare neurodegenerative prion disease that results in trouble sleeping as its hallmark symptom.
Other symptoms include profuse sweating, miosis (pinpoint pupils), sudden entrance into menopause or impotence, neck stiffness, and elevation of blood pressure and heart rate.
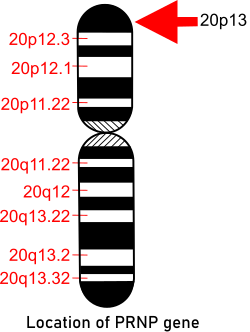
The gene, which provides instructions for making the prion protein PrPC, is located on the short arm of chromosome 20 at position p13.
[11] Individuals with FFI or familial Creutzfeldt–Jakob disease (fCJD) both carry a mutation at codon 178 of the prion protein gene.
[12] FFI is an autosomal dominant disease caused by a missense GAC-to-AAC mutation at codon 178 of the PRNP prion protein gene located on chromosome 20, along with the presence of the methionine polymorphism at position 129 of the mutant allele.
The extent of this symptom varies between two variations of the disease, these being those presenting methionine homozygotes at codon 129 and methionine/valine heterozygotes, with some evidence that hypo-metabolism is more severe in the latter.
[16][17] Diagnosis is based on symptoms and can be supported by a sleep study, a PET scan and genetic testing if the patient's family has a history of the disease.
A test that measures the cerebral metabolic rate of glucose by positron emission tomography (PET), referred to as [18F]-FDG-PET, has demonstrated severe hypometabolism of the thalamus bilaterally in FFI and sFI, also in the earliest stages of the disease.
In 1998 40 families were known to carry the gene for FFI globally: eight German, five Italian, four American, two French, two Australian, two British, one Japanese and one Austrian.
[29] In late 1983 Italian neurologist/sleep expert Dr Ignazio Roiter received a patient at the University of Bologna hospital's sleep institute.
At the time, a prion disease was not suspected due to a lack of prion-related histpathology and frozen brain tissue for advanced analysis.
[Medori et al. NEJM, 1992] In an article published in 2006, Schenkein and Montagna wrote of a 52-year-old American man who was able to exceed the average survival time by nearly one year with various strategies that included vitamin therapy and meditation, different stimulants and hypnotics and even complete sensory deprivation in an attempt to induce sleep at night and increase alertness during the day.
He managed to write a book and drive hundreds of miles in this time, but nonetheless, over the course of his trials, the man succumbed to the classic four-stage progression of the illness.
The man came in with symptoms of double vision and progressive memory loss, and his family also noted he had recently become disoriented, paranoid and confused.
[26] Still with unclear benefit in humans, a number of treatments have had tentative success in slowing disease progression in animal models, including pentosan polysulfate, mepacrine, and amphotericin B.
[32] These mice appear to have progressively fewer and shorter periods of uninterrupted sleep, damage in the thalamus, and early deaths, similar to humans with FFI.
Other research interests involve identifying biomarkers to track the progression of prion disease in living people.