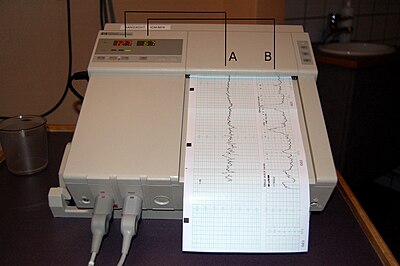
Cardiotocography
Modern-day CTG was developed and introduced in the 1950s and early 1960s by Edward Hon, Roberto Caldeyro-Barcia and Konrad Hammacher.
[1] CTG monitoring is widely used to assess fetal well-being by identifying babies at risk of hypoxia (lack of oxygen).
[3][4] A review found that in the antenatal period (before labour), there is no evidence to suggest that monitoring women with high-risk pregnancies benefits the mother or baby, although research around this is old and should be interpreted with caution.
[5] A study found that CTG monitoring didn't significantly improve or worsen the outcome, in terms of preventable child death, post birth mortality, of pregnancy for high risk mothers.
The absolute values of pressure readings on an external tocometer are dependent on position and are not sensitive in people who are obese.
Combined with an internal fetal monitor, an IUPC may give a more precise reading of the baby's heart rate and the strength of contractions.
A variety of systems for centralized viewing of CTG have been installed in maternity hospitals in industrialised countries, allowing simultaneous monitoring of multiple tracings in one or more locations.
This nomenclature has been adopted by the Association of Women's Health, Obstetric and Neonatal Nurses (AWHONN), the American College of Obstetricians and Gynecologists (ACOG), and the Society for Maternal-Fetal Medicine.
The NICHD nomenclature[14] defines uterine activity by quantifying the number of contractions present in a 10-minute window, averaged over 30 minutes.
According to the International Federation of Gynaecology and Obstetrics (FIGO), a saltatory pattern is defined as FHR baseline amplitude changes of more than 25 bpm with durations of >30 minutes.
[25] In a recently published large obstetric cohort study of the zigzag pattern in almost 5,000 term deliveries in Helsinki University Central Hospital, Tarvonen et al. (2020)[19] reported: "ZigZag pattern and late decelerations of FHR were associated with cord blood acidemia, low Apgar scores, need for intubation and resuscitation, NICU admission and neonatal hypoglycemia during the first 24 hours after birth."
[25][27] It has been linked with rapidly progressing hypoxia,[29] for example due to an umbilical cord compression, and it is presumed to be caused by an instability of the fetal central nervous system.
In a study by Tarvonen et al. (2019),[20] it was demonstrated that the occurrence of saltatory pattern (already with the minimum duration of 2 minutes) in CTG tracings during labor was associated with fetal hypoxia indicated by high umbilical vein (UV) blood erythropoietin (EPO) levels and umbilical artery (UA) blood acidosis at birth in human fetuses.
[20] Due to a standardized terminology and to avoid miscommunication on CTG interpretation, it has been recently proposed in an exhaustive BJOG review of animal and human studies that terms such as saltatory pattern, ZigZag pattern and marked variability should be abandoned, and the common term "increased variability" should be used in clinical CTG guidelines.
[14] FIGO has recently modified the guidelines on intrapartum fetal monitoring, proposing the following interpretation:[35] According to the Cochrane review from February 2017, CTG was associated with fewer neonatal seizures but it is unclear if it had any impact on long-term neurodevelopmental outcomes.
The authors see the challenge in how to discuss these results with women to enable them to make an informed decision without compromising the normality of labour.