Prenatal testing
It is complemented in some regions of the United States, as the Quad test (adding inhibin A to the panel, resulting in an 81% sensitivity and 5% false-positive rate for detecting Down syndrome when taken at 15–18 weeks of gestational age).
[26] In vanishing twin pregnancies with a second gestational sac with a dead fetus, first-trimester screening should be based solely on the maternal age and the nuchal translucency scan as biomarkers are altered in these cases.
[27][28] Computational predictive model shows that extensive and diverse feto-maternal protein trafficking occurs during pregnancy and can be readily detected non-invasively in maternal whole blood.
Entering fetal gene transcripts previously identified in maternal whole blood into a computational predictive model helped develop a comprehensive proteomic network of the term neonate.
It also shows that the fetal proteins detected in pregnant woman's blood originate from a diverse group of tissues and organs from the developing fetus.
In a study published in the March 6, 2011, online issue of Nature, using this non-invasive technique a group of investigators from Greece and UK achieved correct diagnosis of 14 trisomy 21 (Down syndrome) and 26 normal cases.
[32] With commercially available non-invasive (blood) testing for Down syndrome having become available to patients in the United States and already available in China, in October 2011, the International Society for Prenatal Diagnosis created some guidance.
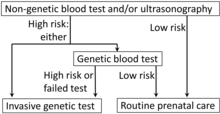
[34] The goal of prenatal genetic testing is to identify pregnancies at high risk of abnormalities, allowing for early intervention, termination or appropriate management and preparation measures.
[44] Carrier screening is a general DNA test that uses a blood or cheek swab sample to determine if the parents carry certain genetic conditions.
[47] Previous studies found elevated levels of acellular placental DNA for trisomy 13 and 21 from maternal serum when compared to women with euploid pregnancies.
[48] Circulating placental nucleated cells comprise only three to six percent of maternal blood plasma DNA, reducing the detection rate of fetal developmental abnormalities.
This test looks at a specific protein that is formed in the liver of the fetus and released into the fluid contents of the womb, which is then absorbed into the mother's blood stream.
A tissue cell sample of the placenta is obtained abdominally via needle or via vaginal insertion of a catheter/syringe into the cervix in combination with ultrasound to guide the procedure.
[52] Amniocentesis is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or neural tube abnormalities.
[52] PUBS is an invasive diagnostic test that can be done during the second trimester of pregnancy for individuals that are looking to identify or are at higher risk of passing chromosomal and/or blood abnormalities.
The procedure is typically done via needle into the mother's abdomen, in combination with ultrasound for guidance, to obtain a blood sample from the umbilical cord of the fetus.
[53] A variation of the PCR technique called multiplex ligation-dependent probe amplification (MLPA), targeting DNA, has been successively applied for diagnosing fetal aneuploidy as a chromosome- or gene-specific assay.
One study comparing transabdominal chorionic villus sampling with second trimester amniocentesis found no significant difference in the total pregnancy loss between the two procedures.
[57][58] The American College of Obstetricians and Gynecologists (ACOG) guidelines currently recommend that anyone who is pregnant, regardless of age, should discuss and be offered non-invasive prenatal genetic screening and diagnostic testing options.
[62] After comprehensive counseling and discussion that acknowledges residual risks, it is important to respect the patients' right of choosing whether or not to pursue any component of genetic testing.
[citation needed] The following are some reasons why a woman might consider her risk of birth defects already to be high enough to warrant skipping screening and going straight for invasive testing:[61] Research was conducted to determine how women felt about noninvasive diagnosis of fetal aneuploid using maternal blood.
[80] Article L2131-1 of the Public Health Code, stemming from the July 2011 bioethics law, states that "prenatal diagnosis refers to medical practices, including obstetric and fetal ultrasound, aimed at detecting, in utero, a particularly severe condition in the embryo or fetus."
The law requires that pregnant women receive clear information about these techniques to "assess the risk that the embryo or fetus may have a condition that could alter the course or management of the pregnancy.
Ultrasound results may also show "soft signs," such as an Echogenic intracardiac focus or a Choroid plexus cyst, which are usually normal, but can be associated with an increased risk for chromosome abnormalities.
5% was the rate quoted in the large clinical studies that were done by the best researchers and physicians, where all the ultrasounds were done by well-trained sonographers and the gestational age of the fetus was calculated as closely as possible.
In the real world, where calculating gestational age may be a less precise art, the formulas that generate a patient's risk score are not as accurate and the false-positive rate can be higher, even 10%.
A patient who received a 1:330 risk score, while technically low-risk (since the cutoff for high-risk is commonly quoted as 1:270), might be more likely to still opt for a confirmatory invasive test.
Many maternal-fetal specialists do not bother to even do an AFP test on their patients because they do a detail ultrasound on all of them in the 2nd trimester, which has a 97% detection rate for neural tube defects such as anencephaly and open spina bifida.
In one case a man who was born with spina bifida was awarded $2 million in settlement, apart from medical expenses, due to the OBGYN's negligence in conducting AFP tests.
[citation needed] Early diagnosis gives the parents time to research and discuss post-natal treatment and care, or in some cases, abortion.