Hysterectomy
[1] It is expected that the frequency of hysterectomies for non-malignant indications will continue to fall given the development of alternative treatment options.
Because of this, hysterectomy is normally recommended as a last resort after pharmaceutical or other surgical options have been exhausted to remedy certain intractable and severe uterine/reproductive system conditions.
Such conditions and/or indications include, but are not limited to:[3] In 1995, the short-term mortality (within 40 days of surgery) was reported at 0.38 cases per 1000 when performed for benign causes.
Women under the age of 45 years have a significantly increased long-term mortality that is believed to be caused by the hormonal side effects of hysterectomy and prophylactic oophorectomy.
Surprisingly, a similar and only slightly weaker effect has been observed for endometrial ablation which is often considered as an alternative to hysterectomy.
The picture is significantly different for hysterectomy performed for malignant reasons; the procedure is often more radical with substantial side effects.
[29] One study showed that risk of subsequent cardiovascular disease is substantially increased for women who had hysterectomy at age 50 or younger.
Those who have undergone a hysterectomy with both ovaries removed typically have reduced testosterone levels as compared to those left intact.
[35] Urinary incontinence and vaginal prolapse are well known adverse effects that develop with high frequency a very long time after the surgery.
One long-term study found a 2.4 fold increased risk for surgery to correct urinary stress incontinence following hysterectomy.
The risk is increased by obesity, diabetes, immunodeficiency disorder, use of systemic corticosteroids, smoking, wound hematoma, and preexisting infection such as chorioamnionitis and pelvic inflammatory disease.
The recommended treatment of an incisional abscess after hysterectomy is by incision and drainage, and then coverage by a thin layer of gauze followed by sterile dressing.
In addition, it is recommended to administer an antibiotic active against staphylococci and streptococci, preferably vancomycin when there is a risk of MRSA.
Alternatively, if the infection is cleared and healthy granulation tissue is evident at the base of the wound, the edges of the incision may be reapproximated, such as by using butterfly stitches, staples or sutures.
[50] Depending on the indication there are alternatives to hysterectomy: Levonorgestrel intrauterine devices are highly effective at controlling dysfunctional uterine bleeding (DUB) or menorrhagia and should be considered before any surgery.
A mass of microspheres or polyvinyl alcohol (PVA) material (an embolus) is injected into the uterine arteries in order to block the flow of blood through those vessels.
[57] Uterine fibroids can be removed with a non-invasive procedure called Magnetic Resonance guided Focused Ultrasound (MRgFUS).
These include, but are not limited to, use of "kegel exercises", vaginal pessary, constipation relief, weight management, and care when lifting heavy objects.
The principal disadvantage is that risk of cervical cancer is not eliminated and women may continue cyclical bleeding (although substantially less than before the surgery).
These issues were addressed in a systematic review of total versus supracervical hysterectomy for benign gynecological conditions, which reported the following findings:[63] In the short-term, randomized trials have shown that cervical preservation or removal does not affect the rate of subsequent pelvic organ prolapse.
[70] The recovery time for an open hysterectomy is 4–6 weeks and sometimes longer due to the need to cut through the abdominal wall.
An open hysterectomy provides the most effective way to explore the abdominal cavity and perform complicated surgeries.
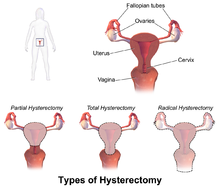
[73][74] Abdominal hysterectomy, the most common method, is used in cases such as after caesarean delivery, when the indication is cancer, when complications are expected, or surgical exploration is required.
With the development of laparoscopic techniques in the 1970s and 1980s, the "laparoscopic-assisted vaginal hysterectomy" (LAVH) has gained great popularity among gynecologists because compared with the abdominal procedure it is less invasive and the post-operative recovery is much faster.
[79] Dual-port laparoscopy is a form of laparoscopic surgery using two 5 mm midline incisions: the uterus is detached through the two ports and removed through the vagina.
[82] Patient characteristics such as the reason for needing a hysterectomy, uterine size, descent of the uterus, presence of diseased tissues surrounding the uterus, previous surgery in the pelvic region, obesity, history of pregnancy, the possibility of endometriosis, or the need for an oophorectomy, will influence a surgeon's surgical approach when performing a hysterectomy.
[87] In another study conducted in 2014, laparoscopy was found to be "a safe alternative to laparotomy" in patients receiving total hysterectomy for endometrial cancer.
Researchers concluded the procedure "offers markedly improved perioperative outcomes with a lower reoperation rate and fewer postoperative complications when the standard of care shifts from open surgery to laparoscopy in a university hospital".
[92] Previously reported marginal advantages of robotic assisted surgery could not be confirmed; only differences in hospital stay and cost remain statistically significant.
[1] Such rates being highest in the industrialized world has led to the controversy that hysterectomies are being largely performed for unwarranted reasons.