Follicular lymphoma
These cells normally occupy the follicles (nodular swirls of various types of lymphocytes) in the germinal centers of lymphoid tissues such as lymph nodes.
The cancerous cells in FL typically form follicular or follicle-like structures (see adjacent Figure) in the tissues they invade.
They may then circulate in the blood to cause an asymptomatic condition termed in situ lymphoid neoplasia of the follicular lymphoma type (i.e. ISFL).
[5] However, recent advancements in the treatment of t-FL (e.g., the addition to standard chemotherapy of agents such as rituximab) have improved overall survival times.
In consequence, multiple B-cell clones that exhibit increasing genomic alterations and malignant behaviors populate the disorder.
This translocation is proposed to occur during the early development of immature bone marrow B-cells (i.e. pre-B-cells/pro-B-cells) after which these cells circulate freely and in rare cases accumulate and mature to centrocytes and/or centroblasts in the germinal centers of lymphoid follicles to form ISFL.
[20] ISFL may also acquire numerous copy-number variations (i.e. duplications and deletions of a portion of a chromosome along with any of the genes contained therein) that may contribute to FL.
[32] FL is commonly preceded by but uncommonly progresses to ISFL, an asymptomatic disorder that usually is discovered in tissues which are biopsied for other reasons.
[10] FL commonly presents as an otherwise asymptomatic enlargement of lymph nodes in the neck, armpit, groin,[13] femoral canal,[33] or other sites in individuals (median age 65) without a known history of ISFL or abnormal numbers of circulating t(14:18)q32:q21-conatianing lymphocytes.
In spite of the evidence of bulky and disseminated disease, predominantly diffuse follicular lymphoma with 1p36 deletion appears to be an indolent disorder that may require long-term observation rather than overtreatment.
[41] The disorder was recently defined by the World Health Organization (2016) as a distinct entity that occurs mostly in males[7] and involves swollen lymph nodes in the head (including tonsils and adenoids), neck,[41] or, rarely, axillary, or inguinal areas, or non-lymphoid tissues.
[41] The lesions in PTFL consists of infiltrates containing rapidly proliferating centrocytes and centroblasts that lack the t(14:18)(q32:q21.3) translocation but nonetheless often overexpress the BCL2 gene.
[45] More than 2 dozen other genes have been reported to be mutated in rare cases of PTFL but in general the genetic abnormalities found in this disorder are fewer and less complex than those in other types of FL.
These FL patients present with the: fast growth of lymph nodes; formation of extra-nodal lesions in extra-nodal sites such as the central nervous system, liver or bone; the onset of B-symptoms (i.e. fever, night sweats, weight loss); development of hypercalcemia (i.e. high serum levels of calcium); and/or sudden rises in serum levels of the enzyme lactate dehydrogenase.
[1] Typically, all the various forms of t-FL are aggressive, rapidly progressive diseases with overall media survival times in treated patients of ~4.5 years.
[49] The diagnosis of FL depends on examining involved tissues for histological, immunological, and chromosomal abnormalities that are indicative of the disease.
FL usually involves enlarged lymph nodes populated by abnormal follicles (see adjacent picture) that when examined histologically contain a mixture of centrocytes or centroblast surrounded by non-malignant cells, mostly T-cells.
None of these protein markers or genomic abnormalities are diagnostic for FL, e.g. the t(14:18)(q32:q21.3) translocation is found in 30% of diffuse large B-cell lymphoma and in a small number of reactive benign lymph nodes.
[1] Other findings indicating the presence of this transformation include rapid growth in size of lymph nodes, recently acquired or new B symptoms, recent development of FL lesions in non-nodal tissue, rapid rises in serum lactate dehydrogenase levels, and the presence of high levels of serum calcium.
Currently used indicators for this include the disease's: 1) histology; 2) subtype; 3) predicted indolence and potential for transformation; and 4) extent of disease as measured by clinical examinations, bone marrow biopsy to determine bone marrow involvement, and PET/CT imaging of the chest, abdomen, pelvis, and any areas outside of these regions if physical examination suggests involvement.
In these cases, which are sometimes classified as Ann Arbor stage I (i.e. disease limited to a single restricted region) or stage II (i.e. disease restricted to two sites that are on the same side of the diaphragm),[4] radiation therapy achieves 10 year overall survival rates of 60–80% and median overall survival times of 19 years.
Findings in asymptomatic patients who have been recommended as triggers for starting treatment include one or more of the following: tumor size ≥7 cm in diameter; involvement of ≥3 nodes in 3 distinct areas, each of which is ≥3 cm in diameter; organ compression; presence of ascites or pleural effusion (i.e. build-up of fluid in the abdominal or pleural cavities); poor performance status due to the disease; elevated levels of serum lactose dehydrogenase or beta-2 microglobulin;[4] presence of localized bone lesions; kidney involvement; reduced levels of circulating blood platelets or any of the various types of white blood cells; onset of significant pruritus (i.e. itching sensation) or other B symptoms; and enlargement (i.e. ≥50% increase in size over a period of at least 6 months) of lymph nodes, spleen, or other follicular lymphoma-infiltrated organs or tissues.
Newer agents used to treat FL include monoclonal antibodies such as rituximab, obinutuzumab, galiximab, inotuzumab ozogamicin, or epratuzumab and immunomodulators such as lenalidomide and interferon.
[13] Finally, surgery[55][56] and radiation[4][13][33] are additional therapies that can be used to relieve symptoms caused by bulky t-FL disease or to treat lesions in patients who cannot withstand other types of treatment.
Early studies on treating t-FL with various purely chemotherapy regimens gave poor results with median overall survival times of 1–2 years.
However, the addition of rituximab to the regimens such as CVP and CHOP as part of induction and maintenance therapies (i.e. R-CVP and R-CHOP) greatly improved overall 5 year survival to rates of 73%.
[5] However, these regimens need not be started in people with FL who are asymptomatic and have low tumor burdens: the outcomes in such patients show no difference between early versus delayed treatment.
[4] Several studies, while not conclusive, suggest that the early treatment of low risk FL reduces the incidence of the disease progressing to t-FL.
While studies are inconclusive, autologous stem cell bone marrow transplantation appears to prolong survival in early treatment failure patients who are healthy enough to withstand this therapy.
[13] Other mostly experimental treatments currently under study in patients with multiple treatment failures include: 1) Phosphoinositide 3-kinase inhibitors such as copanlisib, duvelisib, and idelalisib which block the phosphoinositide 3-kinase signaling pathway that promotes the survival, proliferation, and other potentially malignant behaviors of cells; 2) infusion of tisagenlecleucel chimeric antigen receptor T cells (i.e.

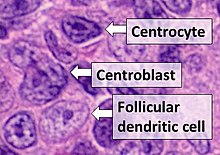
- Centrocytes are small to medium size with angulated, elongated, cleaved, or twisted nuclei.
- Centroblasts are larger cells containing vesicular nuclei with one to three basophilic nucleoli apposing the nuclear membrane.
- Follicular dendritic cells have round nuclei, centrally located nucleoli, bland and dispersed chromatin, and flattening of adjacent nuclear membrane.
