Parkinsonian gait
[4][5][6] Patients with PD demonstrate reduced stride length, walking speed during free ambulation and cadence rate, while double support duration is increased.
In addition, PD patients have reduced foot lifting during the swing phase of gait, which produces smaller clearance between the toes and the ground.
The intra-individual variability in foot strike pattern is found to be surprisingly lower in PD patients compared with those with a typical gait.
[15][16] In the earlier stages of the disease, reduced forces (or peak heights) are found for heel contact and the push-off phase resembling that of elderly subjects.
In the more advanced stages of the disorder where gait is characterized by small shuffling steps, PD patients show only one narrow peak in the vertical GRF signal.
[19] Current treatments for FOG offer only limited benefits but a range of novel approaches are being actively explored,[20] and thought is being given to how future research strategies are best coordinated.
[21] The most common form of FOG is 'start hesitation' (which happens when the patient wants to start walking) followed in frequency by 'turning hesitation'[22][23] FOG can also be experienced in narrow or tight quarters such as a doorway, whilst adjusting one's steps when reaching a destination, and in stressful situations such as when the telephone or the doorbell rings or when the elevator door opens.
[17] It is proven that psychological interventions can help reduce negative effect of psychosocial factors, like anxiety or depression, that can worsen freezing of gait or tremor in Parkinson's patients.
Falls result mainly due to sudden changes in posture, in particular turning movements of the trunk, or attempts to perform more than one activity simultaneously with walking or balancing.
[17] Falls that occur frequently very early in the disease course may signify that another diagnosis (such as progressive supranuclear palsy) should be considered.
[25] Postural instability in upright stance is common in end-stage PD and compromises the ability to maintain balance during everyday tasks such as walking, turning and standing up from sitting.
[28] This implies that PD patients have higher passive stiffness of ankle joints, show larger background EMG activity and more co-contraction of leg muscles in stance.
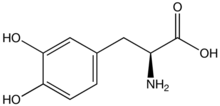
L-dopa is able to pass the blood–brain barrier as a prodrug and is decarboxylated in the brain to the neurotransmitter dopamine by the enzyme aromatic-L-amino-acid decarboxylase.
[35] Basal ganglia dysfunction in PD causes it to stop acting as an internal cue for gait in Parkinson's patients.
[36] In addition gait initiation has been shown to be significantly improved in PD patients compared with auditory cues.
Deep brain stimulation (DBS) in the pedunculopontine nucleus, a part of the brainstem involved in motor planning,[41] has been shown to improve gait function in patients with Parkinson's disease.
[42] DBS in the subthalamic nucleus (STN) and the globus pallidus have also been shown to have positive effects on gait abnormalities presented by Parkinson's Disease patients.
The therapist may also use tiles or footprints on the ground to improve foot placement and widen the patient's base of support.
[49] Creative visualization of walking with a more normalized gait pattern, and mentally rehearsing the desired movement has also shown to be effective.
However, through regression analysis studies have revealed that in Parkinson's, increasing the velocity of walking changes the stride length linearly (which resembles that of controls).