Glucagon-like peptide-1
Endogenous GLP-1 is rapidly degraded primarily by dipeptidyl peptidase-4 (DPP-4), as well as neutral endopeptidase 24.11 (NEP 24.11) and renal clearance, resulting in a half-life of approximately 2 minutes.
The proglucagon gene is expressed in several organs including the pancreas (α-cells of the islets of Langerhans), gut (intestinal enteroendocrine L-cells) and brain (caudal brainstem and hypothalamus).
In mammals, the transcription gives rise to identical mRNA in all three cell types, which is further translated to the 180 amino acid precursor called proglucagon.
[3] In the gut and brain, proglucagon is catalysed by PC 1/3 giving rise to glicentin, which may be further processed to GRPP and oxyntomodulin, GLP-1, intervening peptide-2 (IP-2) and glucagon-like peptide-2 (GLP-2).
[3][4] GLP-1 is packaged in secretory granules and secreted into the hepatic portal system by the intestinal L-cells located primarily in the distal ileum and colon, but also found in the jejunum and duodenum.
The L-cells are open-type triangular epithelial cells directly in contact with the lumen and neuro-vascular tissue and are accordingly stimulated by various nutrient, neural and endocrine factors.
As the majority of L-cells are located in the distal ileum and colon, the early phase is likely explained by neural signalling, gut peptides or neurotransmitters.
Other evidence suggests the L-cells located in the proximal jejunum are sufficient to account for the early-phase secretion through direct contact with luminal nutrients.
The rate of gastric emptying is therefore an important aspect to consider, as it regulates the entry of nutrients into the small intestine where the direct stimulation occurs.
[1][2] Fasting plasma concentrations of biologically active GLP-1 range between 0 and 15 pmol/L in humans and are increased 2- to 3-fold upon food consumption depending on meal size and nutrient composition.
Sugars have been associated with various signalling pathways, which initiate depolarisation of the L-cell membrane causing an elevated concentration of cytosolic Ca 2+, which in turn induces GLP-1 secretion.
[3] Neutral endopeptidase 24.11 (NEP 24.11) is a membrane-bound zinc metallopeptidase widely expressed in several tissues, but found in particularly high concentrations in the kidneys, which is also identified accountable for the rapid degradation of GLP-1.
It primarily cleaves peptides at the N-terminal side of aromatic or hydrophobic amino acids and is estimated to contribute by up to 50% to GLP-1 degradation.
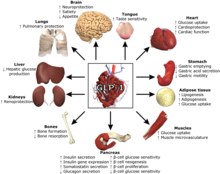
GLP-1 possesses several physiological properties making it (and its functional analogs) a subject of intensive investigation as a potential treatment of diabetes mellitus, as these actions induce long-term improvements along with the immediate effects.
[14] GLP-1 has also shown signs of carrying out protective and regulatory effects in numerous other tissues, including heart, tongue, adipose, muscles, bones, kidneys, liver and lungs.
[citation needed] In the early 1980s, Richard Goodman and P. Kay Lund were postdoctoral researchers working in Joel Habener's laboratory at Massachusetts General Hospital.