Glycogen storage disease
[2] However, not every inborn error of carbohydrate metabolism has been assigned a GSD number, even if it is known to affect the muscles or liver.
Ischemia that often produces symptoms in the leg muscles includes intermittent claudication, popliteal artery entrapment syndrome, and chronic venous insufficiency.
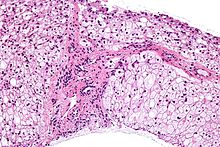
[56] In patients with increased growth hormone, muscle biopsy includes, among other features, excess glycogen deposition.
[80] DMD-related childhood-onset milder phenotypes present with exercise-induced muscle cramping, stiffness, pain, fatigue, and elevated CK.
[81] Becker muscular dystrophy has adult-onset exercise-induced muscle cramping, pain, and elevated CK.
[87] Dimethylglycine dehydrogenase deficiency has muscle fatigue, elevated CK, and fishy body odour.
[89] (help wikipedia by contributing to this subsection) Glycogenosis-like phenotype of congenital hyperinsulinism due to HNF4A mutation or MODY1 (maturity-onset diabetes of the young, type 1).
This phenotype of MODY1 has macrosomia and infantile-onset hyperinsulinemic hypoglycemia, physiological 3-OH butyrate, increased triglyceride serum levels, increased level of glycogen in liver and erythrocytes, increased liver transaminases, transient hepatomegaly, renal Fanconi syndrome, and later develop liver cirrhosis, decreased succinate-dependent respiration (mitochondrial dysfunction), rickets, nephrocalcinosis, chronic kidney disease, and diabetes.
Von Gierke disease (GSD-I) is typically treated with frequent small meals of carbohydrates and cornstarch, called modified cornstarch therapy, to prevent low blood sugar, while other treatments may include allopurinol and human granulocyte colony stimulating factor.
[93] Cori/Forbes disease (GSD-III) treatment may use modified cornstarch therapy, a high protein diet with a preference to complex carbohydrates.
However, unlike GSD-I, gluconeogenesis is functional, so simple sugars (sucrose, fructose, and lactose) are not prohibited.
[94][95] For phosphoglucomutase deficiency (formerly GSD-XIV), D-galactose supplements and exercise training has shown favourable improvement of signs and symptoms.
[45][60][96][97] Studies have shown that regular low-moderate aerobic exercise increases peak power output, increases peak oxygen uptake (V̇O2peak), lowers heart rate, and lowers serum CK in individuals with McArdle disease.
[97][98] For the regularly active patients, it took more strenuous exercise (very brisk walking/jogging or bicycling) for them to experience both the typical symptoms and relief thereof, along with the sign of an increased heart rate dropping, demonstrating second wind.
[97][98][99] In young children (<10 years old) with McArdle disease (GSD-V), it may be more difficult to detect the second wind phenomenon.
"[45][60][102] However, they can achieve sub-maximal benefit from lipid metabolism of free fatty acids during aerobic activity following a warm-up.
[45] Overall, according to a study in British Columbia, approximately 2.3 children per 100,000 births (1 in 43,000) have some form of glycogen storage disease.