HIV and pregnancy
Notably, without antiretroviral medications, obstetrical interventions, and breastfeeding recommendations, there is approximately a 30% risk of mother-to-child HIV transmission.
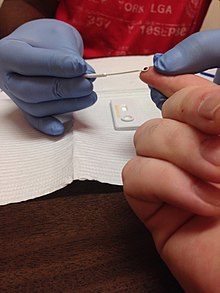
[5] The American College of Obstetrics and Gynecology (ACOG) therefore recommends HIV testing as a routine component of both pre-pregnancy and first trimester prenatal care to ensure expedient and appropriate interventions.
Notably, 20-34% of women in the United States living with HIV are unaware of their diagnosis until they become pregnant and undergo prenatal screening.
It is thought that mother-to-child HIV transmission most commonly occurs at the time of delivery when the baby comes into direct contact with the mother's infected blood or genital secretions/fluid in the birth canal.
If symptoms develop, the most common include persistent fevers, generalized lymph node swelling, enlarged spleen and/or liver, growth failure, and diarrhea.
[12] ACOG and the National Institutes of Health (NIH) recommends all couples in which one or both partners are HIV positive seek pre-pregnancy counseling and consult experts in Obstetrics and Gynecology, Infectious Disease, and possibly reproductive endocrinology and infertility to ensure couples are getting appropriate, individualized guidance based on their specific disease states and weighing the risks to the fetus associated with taking ART medications.
[14] The NIH advises administering PrEP to serodiscordant couples who are going to attempt conception via condomless sex, however, they emphasize that adherence is absolutely necessary to effectively protect the HIV negative partner.
When the female attempting to conceive is HIV positive, she can undergo assisted insemination with semen from her partner to reduce the risk of transmission.
[6][19] The CDC, NIH, ACOG, and American Academy of Pediatrics each recommend first trimester HIV testing for all pregnant women as a part of routine prenatal care.
[7][1] The NIH further elaborates on this recommendation, indicating that HIV testing should be conducted as early as possible wherever a woman seeks care and initially determines she is pregnant (for example, in the Emergency Department).
For this reason, ART is recommended throughout the pregnancy so that viral load levels remain as low as possible and the risk of transmission is reduced.
The recommendation is stronger in the following situations:[34] Women should continue taking their ART regimen on schedule and as prescribed throughout both the prenatal period and childbirth.
IV Zidovudine is only not administered if women are both compliant with their prescribed ART regimen throughout pregnancy and have maintained a low viral load near the time of delivery (HIV RNA less than 50 copies/mL between 34 and 36 weeks gestation).
[36] Vaccination is important to prevent serious infectious complications associated with the aforementioned diseases, which patients with HIV are at higher risk of contracting.
[37] The following monitoring tests are recommended for women who are diagnosed with HIV prior to or during pregnancy:[38] The goals of antiretroviral administration during pregnancy are to reduce the risk of transmission of HIV from mother to child, to slow maternal disease progression, and to reduce the risks of maternal opportunistic infection and death.
[12] Vitamin A plays a role in the immune system and has been suggested as a low-cost intervention that could help with preventing mother-to-child transmission of HIV.
[45] Furthermore, high doses of natural Vitamin A can be toxic to the fetus, which is important to consider in management of HIV in pregnant women.
All mothers should continue their antiretroviral medications following hospital discharge, and any changes to their regimens should be made in consultation with the physicians who coordinate their HIV care.
The NIH also advises that providers should be wary of the unique challenges to medication compliance that mothers face in the postpartum period when designing a discharge ART regimen for their patients.
The infant should then be followed with appropriate laboratory monitoring based on their gestational age and clinical condition, and both the fetal and maternal drug regimens.
For these reasons, the NIH, CDC, and the AAP each discourage breastfeeding amongst HIV-positive women in the United States and other developed nations because there are safe, affordable feeding alternatives and clean drinking water.
In these situations, it is important that mothers adhere strictly to their ART regimens and it is advised that infants are administered antiretroviral drugs for the prevention of possible viral transmission for at least 6 weeks.
[55] In developing nations, clean water and formula are not as readily available, therefore, breastfeeding is often encouraged to provide children with adequate food and nutrients because the benefit of nourishment outweighs the risk of HIV transmission.
"[58][33]:95-6 A mother should only give infant formula, as explained by the WHO, if the following conditions are met:[59] Despite advances made in preventing transmission, HIV-positive women still face discrimination regarding their reproductive choices.
[63][64][65] women are forced to undergo sterilisation without their knowledge or informed consent, and misinformation and incentives are often used in order to coerce them into accepting the procedure.
In Namibia, litigation was brought against the government by three HIV-positive women who claimed they were coerced during labour into signing consent forms that gave permission for the hospital to perform a sterilisation.
[68] A 2010 case in Chile have also aimed to seek government accountability for violation of sexual and reproductive rights of women living with HIV.
[72][73] For example, a study of Florida births from 1998 to 2007 showed parents who were identified as Hispanic or Black in the medical records were more likely to have HIV during pregnancy.
[74][75][76] Furthermore, there are large disparities in access to antiretroviral therapies, medications important in preventing the transmission of HIV from parent to child.
[78] There is also research showing that support groups, in the short term, have a significant positive impact for pregnant women living with HIV.