HPV vaccine
[20] In the United States, the Centers for Disease Control and Prevention (CDC) recommends that all 11- to 12-year-olds receive two doses of HPV vaccine, administered 6 to 12 months apart.
[76] On 9 September 2009, an advisory panel recommended that the Food and Drug Administration (FDA) of the USA license Gardasil in the United States for boys and men ages 9–26 for the prevention of genital warts.
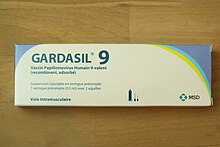
[83] In 2018, the US Food and Drug Administration (FDA) released a summary basis for regulatory action and approval for expansion of usage and indication for Gardasil 9, the 9-valent HPV vaccine, to include men and women 27 to 45 years of age.
[88] In more developed countries, populations that do not receive adequate medical care, such as the poor or minorities in the United States or parts of Europe also have less access to cervical screening and appropriate treatment, and are similarly more likely to benefit.
[108] Gardasil and Cervarix are designed to elicit virus-neutralizing antibody responses that prevent initial infection with the HPV types represented in the vaccine.
[109] In 1983, Harald zur Hausen culminated decades of research with the discovery that certain variants of human papillomaviruses (HPVs) could be found in a majority of tested cervical cancer specimens.
[110] In 1990, Ian Frazer partnered with Jian Zhou and Xiao-Yi Sun at the University of Queensland in Australia to create synthetic HPVs for study in the lab.
[116] Harald zur Hausen was awarded half of the $1.4 million Nobel Prize in Medicine in 2008 for his work showing that cervical cancer is caused by certain types of HPVs.
[118] As of 2013[update], vaccinating girls and young women was estimated to be cost-effective in the low and middle-income countries, especially in places without organized programs for screening cervical cancer.
[132] In May 2013 the Minister of Health of South Africa, Aaron Motsoaledi, announced the government would provide free HPV vaccines for girls aged 9 and 10 in the poorest 80% of schools starting in February 2014 and the fifth quintile later on.
[135] By 2017, HPV coverage data on the Immunise Australia website show that by 15 years of age, over 82% of Australian females had received all three doses.
[135] A 2011 report published found the diagnosis of genital warts (caused by HPV types 6 and 11) had also decreased in young women and men.
In November 2011, the Pharmaceutical Benefits Advisory Committee (PBAC) recommended the extension of the National HPV Vaccination Program to include males.
The PBAC made its recommendation on the preventive health benefits that can be achieved, such as a reduction in the incidence of anal and penile cancers and other HPV-related diseases.
As part of the Hong Kong Childhood Immunisation Programme, HPV vaccines became mandatory for students in the 2019/2020 school year, exclusively for females at primary 5 and 6 levels.
[181] In 2024, the HPV vaccine drive was announced by Finance Minister Nirmala Sitharaman as part of Nari Shakti ("Women Power") campaign but hasn't been implemented yet.
[193][194] In December 2021, the Ministry of Health, Labour and Welfare has decided to allow free vaccines to women born between fiscal year 1997 and 2005 after eight-year hiatus.
The vaccine was initially offered only to girls, usually through a school-based program in Year 8 (approximately age 12), but also through general practices and some family planning clinics.
Since 2016, HPV vaccination has been part of the National Immunization Program, offered free of charge to all children under 12 in South Korea, with costs fully covered by the Korean government.
But was suspended later on that year owing to objections and concerns raised by the Catholic Board, but fully available in local health centers.
[128] Between July 2008 and December 2009, proof of the first of three doses of HPV Gardasil vaccine was required for women ages 11–26 intending to legally enter the United States.
[252] Merck's Vaccine Patient Assistance Program 1-800-293-3881[253] provides Gardasil free to low-income women and men, ages 19 to 26, who do not have insurance, including immigrants who are legal residents.
A review of nearly 1,400 adolescent girls found no difference in teen pregnancy, incidence of sexually transmitted infection, or contraceptive counseling regardless of whether they received the HPV vaccine.
[255] A disproportionate rate of HPV-related cancers exists amongst LatinX populations, leading researchers to explore how communication and messaging can be adjusted to address vaccine hesitancy.
[266] Christine Peterson, director of the University of Virginia's Gynecology Clinic, said "The presence of seat belts in cars doesn't cause people to drive less safely.
Countries have taken different routes based on economics and social climate leading to issues of forced vaccination and marginalization of segments of the population in some cases.
These arguments are supported by World Health Organization (WHO) surveys showing the effectiveness of cervical cancer prevention with HPV vaccination.
[276][277] There is also substantial research interest in the development of therapeutic vaccines, which seek to elicit immune responses against established HPV infections and HPV-induced cancers.
[282][283][284][285] Therapeutic DNA vaccine VGX-3100, which consists of plasmids pGX3001 and pGX3002, has been granted a waiver by the European Medicines Agency for pediatric treatment of squamous intraepithelial lesions of the cervix caused by HPV types 16 and 18.
[291] In 2017, National Cancer Institute scientists Douglas R. Lowy and John T. Schiller received the Lasker-DeBakey Clinical Medical Research Award for their contributions leading to the development of HPV vaccines.