Health care in Australia
State and territory governments operate public health facilities where eligible patients receive care free of charge.
Australian citizens, permanent residents, and some visitors and visa holders are eligible for health services under the Medicare system.
[3] In 2009 before means testing was introduced, the private health insurance rebate was estimated to cost $4 billion, around 20% of the total budget.
[6][7] State and territory governments (through agencies such as Queensland Health) regulate and administer the major elements of healthcare such as doctors, public hospitals and ambulance services.
The NDIS also has supports for family members to aid them in taking care of their loved ones and avoid issues like carer burnout.
[19] Both the MBS and PBS also have "safety nets" which further cover the cost of health care and medicines for people that pay a lot out-of-pocket each year.
Medicare does not cover the cost of ambulance services, most dental care, glasses, contact lenses or hearing aides, and cosmetic surgery.
[21] Families or individuals are also subject to the safety net threshold: after a certain amount of out-of-pocket expenses in a calendar year, Medicare will increase the contribution percentage for specialist services.
[22] Certain concession holders, such as veterans, those with disabilities, and low-income earners receiving payments from Centrelink, often can claim a higher percentage of the scheduled fee than what the general population can.
[22] Other universal health services like the cancer screening programs and the National Disability Insurance Scheme (NDIS) are covered under separate agreements between the different levels of government.
Block funding is specific to each hospital, and is used to cover the cost of teaching and research, and for most rural and remote health facilities.
These sites operate on a commission-basis agreement with their participating health funds and allow consumers to compare policies before joining online.
[32] The ombudsman publishes an annual report that outlines the number and nature of complaints per health fund compared to their market share.
It would also attract people with existing medical conditions, who might not otherwise have taken out insurance at all because of the denial of benefits for 12 months due to the PEA Rule.
The benefits paid out for these conditions would create pressure on premiums for all the fund's members, causing some to drop their membership, which would lead to further rises, and a vicious cycle would ensue.
[citation needed] Health funds are not permitted to discriminate between members in terms of premiums, benefits or membership on the basis of racial origin, religion, sex, sexual orientation, nature of employment, and leisure activities.
The Howard Coalition government introduced a Medicare levy surcharge (MLS) with effect from 1 July 1997, as an incentive for people on higher incomes to take out and maintain an appropriate level of private health insurance,[35] as part of an effort to reduce demand pressure on public hospitals by encouraging people to have insurance cover for them to use private hospitals.
Controversial issues include: Critics argue that the rebate is an unfair subsidy to those who can afford health insurance, claiming the money would be better spent on public hospitals where it would benefit everyone.
To arrest the decline in the number of Australians maintaining private health insurance, the government introduced the Lifetime Health Cover loading, under which people who take out private hospital insurance later in life pay higher premiums, called a "loading", compared to those who have held coverage since they were younger, and may also be subject to the Medicare levy surcharge.
National Boards set the professional practice standards for each profession, and can apply to state and territory tribunals to suspend or remove health practitioner's registration.
[46] The Royal Flying Doctor Service provides both emergency and primary health care in rural and regional Australia using aircraft.
[48] Heart of Australia provides specialist cardiac and respiratory investigation and treatment services in rural and regional Queensland, particularly mining towns, using specially-equipped large trucks.
Governments, Higher Education and Training, Professions and Employers are also identified as key players in the process of addressing future challenges.
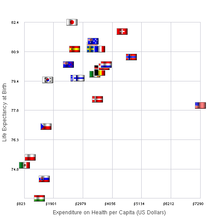
It found that in the healthy lives category, "Australia ranks highest, scoring first or second on all three indicators", although its overall ranking in the study was below the UK and Germany systems, tied with New Zealand's and above those of Canada and far above the U.S.[57][58] A new study published in July 2017 as part of the same 'Mirror, Mirror' series by The Commonwealth Fund compared the health care systems in 11 countries (Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States) and found that Australia was now one of the top ranked countries overall, alongside the United Kingdom and the Netherlands.
In order for the Australian health care system to handle the gradual population aging, government and administration must develop new policies and programs to accommodate the needs of changing demographics.
[21] Data from the Australian Institute of Health and Welfare shows that out-of-pocket payments increased four-and-a-half times faster than government funding in 2014–15.
The introduction of 1- Differential rebating 2- HICAPS and access to members data 3- Patient steering have led to a high level of discontent amongst healthcare providers.
The Australian Dental Association (ADA) set quality and care standards for the industry, but provide no standardised pricing schedule for services and treatment.
The PBS is now administered by the Department of Human Services Insurance, with input from a range of other bodies such as the Pharmaceutical Benefits Pricing Authority.
[71] The National Diabetes Services Scheme is funded by the Australian government to deliver diabetes-related products at affordable prices.