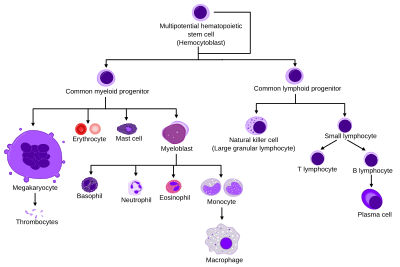
Haematopoiesis
Haematopoiesis (/hɪˌmætəpɔɪˈiːsɪs, ˌhiːmətoʊ-, ˌhɛmə-/;[1][2] from Ancient Greek αἷμα (haîma) 'blood' and ποιεῖν (poieîn) 'to make'; also hematopoiesis in American English, sometimes h(a)emopoiesis) is the formation of blood cellular components.
According to this terminology, the stages of red blood cell formation would be: rubriblast, prorubricyte, rubricyte, metarubricyte, and erythrocyte.
However, the following nomenclature seems to be, at present, the most prevalent: Osteoclasts also arise from hemopoietic cells of the monocyte/neutrophil lineage, specifically CFU-GM.
As development progresses, blood formation occurs in the spleen, liver and lymph nodes.
[13] When bone marrow develops, it eventually assumes the task of forming most of the blood cells for the entire organism.
[3] However, maturation, activation, and some proliferation of lymphoid cells occurs in the spleen, thymus, and lymph nodes.
[15] Extramedullary haematopoiesis and myelopoiesis may supply leukocytes in cardiovascular disease and inflammation during adulthood.
[16][17] Splenic macrophages and adhesion molecules may be involved in regulation of extramedullary myeloid cell generation in cardiovascular disease.
This theory has been supported by experiments showing that within a population of mouse haematopoietic progenitor cells, underlying stochastic variability in the distribution of Sca-1, a stem cell factor, subdivides the population into groups exhibiting variable rates of cellular differentiation.
For example, under the influence of erythropoietin (an erythrocyte-differentiation factor), a subpopulation of cells (as defined by the levels of Sca-1) differentiated into erythrocytes at a sevenfold higher rate than the rest of the population.
In this case, the haematopoietic microenvironment prevails upon some of the cells to survive and some, on the other hand, to perform apoptosis and die.
For example, long-term expression of PU.1 results in myeloid commitment, and short-term induction of PU.1 activity leads to the formation of immature eosinophils.
[29] The first key player of differentiation from HSC to a multipotent progenitor (MPP) is transcription factor CCAAT-enhancer binding protein α (C/EBPα).
[35] Surprisingly, pax5 conditional knock out mice allowed peripheral mature B cells to de-differentiate to early bone marrow progenitors.
[39] In some vertebrates, haematopoiesis can occur wherever there is a loose stroma of connective tissue and slow blood supply, such as the gut, spleen or kidney.

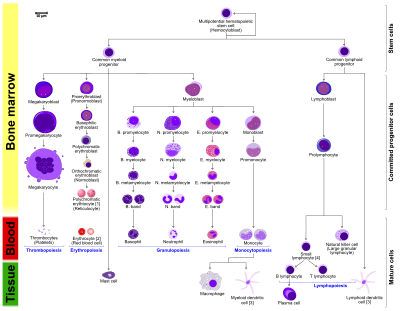
- The morphological characteristics of the hematopoietic cells are shown as seen in a Wright's stain, May-Giemsa stain or May-Grünwald-Giemsa stain. Alternative names of certain cells are indicated between parentheses.
- Certain cells may have more than one characteristic appearance. In these cases, more than one representation of the same cell has been included.
- Together, the monocyte and the lymphocytes comprise the agranulocytes, as opposed to the granulocytes (basophil, neutrophil and eosinophil) that are produced during granulopoiesis.
- B., N. and E. stand for Basophilic, Neutrophilic and Eosinophilic, respectively – as in Basophilic promyelocyte. For lymphocytes, the T and B are actual designations.
- The polychromatic erythrocyte (reticulocyte) at the right shows its characteristic appearance when stained with methylene blue or Azure B.
- The erythrocyte at the right is a more accurate representation of its appearance in reality when viewed through a microscope.
- Other cells that arise from the monocyte: osteoclast, microglia (central nervous system), Langerhans cell (epidermis), Kupffer cell (liver).
- For clarity, the T and B lymphocyte are split to better indicate that the plasma cell arises from the B-cell. Note that there is no difference in the appearance of B- and T-cells unless specific staining is applied.
