History and culture of breastfeeding
[1] During the early 20th century, breastfeeding started to be viewed negatively, especially in Canada and the United States, where it was regarded as a low-class and uncultured practice.
[8] The biologist and physician Linnaeus, the English doctor Cadogan,[9] Rousseau, and the midwife Anel le Rebours[10] described in their writings the advantages and necessity of women breastfeeding their own children and discouraged the practice of wet nursing.
Linnaeus thought that the lower-class wet nurses ate too much fat, drank alcohol and had contagious (venereal) diseases, therefore producing lethal milk.
[17] Dutch historian Van Eekelen researched the small amount of available evidence of breastfeeding practices in The Netherlands.
[22] One of the causes was an increased reliance on pasteurized milk and baby formula products, which were regarded as acceptable substitutes by upwardly mobile mothers.
The practice was considered old-fashioned and "a little disgusting" for those who could not afford infant formula and discouraged by medical practitioners and media of the time.
A 1996 article in the Canadian Journal of Public Health found that, in Vancouver, 82.9% of mothers initiated breastfeeding, but that this differed by Caucasian (91.6%) and non-Caucasian (56.8%) women.
[31] A 2003 La Leche League International study found that 72% of Canadian mothers initiate breastfeeding and that 31% continue to do so past four to five months.
[34] China has implemented many provisions contained in the International Code of Marketing of Breast-milk Substitutes as adopted by the World Health Assembly in 1981.
Breastfeeding in Cuba has been officially recognized and supported by the Cuban government since the 1940 constitution, which included provisions promoting maternal and child health.
It mandates two extraordinary daily rest periods of half an hour each, allowing mothers to breastfeed or express milk for their children while still at work.
This protection aims to facilitate the continuation of breastfeeding even after maternity leave has ended, promoting the health and well-being of both mother and child.
Cuba's efforts to promote breastfeeding are also supported by its robust healthcare infrastructure, which provides free prenatal and postnatal care to all women.
After World War II, Western medicine was taken to Japan and the women began giving birth in hospitals, where the baby was usually taken to the nursery and given formula milk.
[39] However, in a study published in the UK in 2015, a lack of role models such as mothers, other female relatives, and friends who breastfeed was cited as one of the potential barriers for breastfeeding.
[40] Breastfeeding during family gatherings or in the presence of others has also been reported as a challenge for some women from ethnic minority groups in the United Kingdom.
[41][42] In many countries, particularly those with a generally poor level of health, malnutrition is the major cause of death in children under 5, with 50% of all those cases being within the first year of life.
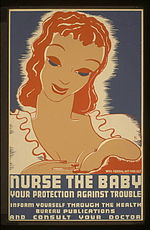
[44][45][46][failed verification] In response to public pressure, the health departments of various governments have recognised the importance of encouraging mothers to breastfeed.
The World Health Organization (WHO), along with grassroots non-governmental organisations like the International Baby Food Action Network (IBFAN) have played a large role in encouraging these governmental departments to promote breastfeeding.
Under this advice they have developed national breastfeeding strategies, including the promotion of its benefits and attempts to encourage mothers, particularly those under the age of 25, to choose to feed their child with breast milk.
The International Code of Marketing of Breast-milk Substitutes was developed in 1981 by WHO, but violations have been reported by organisations, including those networked in IBFAN.
A United States House of Representatives appropriations bill (HR 2490) with a breastfeeding amendment was signed into law on September 29, 1999.
Laws protecting the right to nurse aim to change attitudes and promote increased incidence and duration of breastfeeding.
[49] Despite the legal status, a lack of supportive workplace environments and an inability to express milk have been cited by women as barriers for publicly breastfeeding in the United States.
In California, employers must provide a private, non-bathroom space near the employee's work area for lactation that is safe, clean, and equipped with seating, a surface for personal items, and access to electricity.
Small employers with fewer than 50 employees may be exempt if they demonstrate undue hardship but must still make reasonable efforts to provide a private, nearby space.
The World Health Organization aims to have at least half of all the mothers worldwide exclusively breastfeeding their infants in the first 6 months of life by the year 2025.
A mother holding a very modern-looking nursing bottle in one hand and a stick, presumably to mix the food, in the other is depicted in a relief found in the ruins of the palace of King Ashurbanipal of Nineveh, who died in 888 BC.
[65] The Wabanaki and other Native American tribal nations of North America made an infant formula from nuts and cornmeal.
[citation needed] Though first developed by Henri Nestlé in the 1860s, infant formula received a huge boost during the post–World War II baby boom.