Hyperkinesia
[1] Hyperkinesia is a state of excessive restlessness which is featured in a large variety of disorders that affect the ability to control motor movement, such as Huntington's disease.
[4] Several prominent forms of hyperkinetic movements include: The term ataxia refers to a group of progressive neurological diseases that alter coordination and balance.
Symptoms can range from a simple increased frequency of blinking to constant, painful eye closure leading to functional blindness.
[7] Typically caused by damage to the subthalamic nucleus or nuclei, hemiballismus movements are nonrhythmic, rapid, nonsuppressible, and violent.
[8] Hemifacial spasm (HFS) is characterized by involuntary contraction of facial muscles, typically occurring only on one side of the face.
[7] Myoclonus is defined as a sequence of repeated, often nonrhythmic, brief, shock-like jerks due to sudden involuntary contraction or relaxation of one or more muscles.
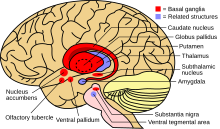
Without the normal restraining influence of the basal ganglia, upper motor neurons of the circuit tend to become more readily activated by inappropriate signals, resulting in the characteristic abnormal movements.
The direct pathway projects to the internal globus pallidus (GPi) and to the substantia nigra pars reticulata (SNr).
This, in turn, causes disinhibition of the STN excitatory outputs, thus triggering the GPi/SNr inhibitory projections to the thalamus and decreased activation of cortical neurons.
[12] Since the basal ganglia often have many connections with the frontal lobe of the brain, hyperkinesia can be associated with neurobehavioral or neuropsychiatric disorders such as mood changes, psychosis, anxiety, disinhibition, cognitive impairments, and inappropriate behavior.
Secondary dystonia, however, is most commonly caused by dyskinetic cerebral palsy, due to hypoxic or ischemic injury to the basal ganglia, brainstem, cerebellum, and thalamus during the prenatal or infantile stages of development.
"Repetitive," "recurrent," and "reciprocal" movements feature a certain bodily or joint position that occur more than once in a period, but not necessarily in a cyclic manner.
It may occur in situations where the individual's motor intention spreads to either nearby or distant muscles, taking away from the original goal of the movement.
The extent of the hyperkinesia exhibited in the disease can vary from solely the little finger to the entire body, resembling purposeful movements but occurring involuntarily.
Caused by the Huntington gene, the disease eventually contributes to selective atrophy of the Caudate nucleus and Putamen, especially of GABAergic and acetylcholinergic neurons, with some additional degeneration of the frontal and temporal cortices of the brain.
Some examples include athetosis, chorea with or without hemiballismus, tremor, dystonia, and segmental or focal myoclonus, although the prevalence of these manifestations after stroke is quite low.
The amount of time that passes between stroke event and presentation of hyperkinesia depends on the type of hyperkinetic movement since their pathologies slightly differ.
Strokes causing small, deep lesions in the basal ganglia, brain stem and thalamus are those most likely to be associated with post-stroke hyperkinesia.
That toward the ventral intermediate nucleus of the thalamus has been shown to reduce contralateral and some ipsilateral tremor along with tremors of the cerebellar outflow, head, resting state and those related to hand tasks; however, the treatment has been shown to induce difficulty articulating thoughts (dysarthria), and loss of coordination and balance in long-term studies.
[15] Treatment of primary dystonia is aimed at reducing symptoms such as involuntary movements, pain, contracture, embarrassment, and to restore normal posture and improve the patient's function.
Anticholinergic drugs prove to be most effective in treating generalized and segmental dystonia, especially if dose starts out low and increases gradually.
[20] Botulinum toxin B, or Myobloc, has been approved by the US Food and Drug Administration to treat cervical dystonia due to level A evidential support by the scientific community.
About a century later, Thomas Willis noticed that the corpus striatum was typically discolored, shrunken, and abnormally softened in the cadavers of people who had died from paralysis.
The view that the corpus striatum played such a large role in motor functions was the most prominent one until the 19th century when electrophysiologic stimulation studies began to be performed.
[23] By the late 19th century, a few hyperkinesias such as Huntington's chorea, post-hemiplegic choreoathetosis, Tourette's syndrome, and some forms of both tremor and dystonia were described in a clinical orientation.
It was not until the late 1980s and 1990s that sufficient animal models and human clinical trials were utilized to discover the specific involvement of the basal ganglia in the hyperkinesia pathology.
Such bursts can occur in multiple muscles simultaneously quite quickly, but high time resolution must be used in the EMG trace to clearly record them.
However, it may be predicted that the EMG for chorea would include bursts varying in duration, timing, and amplitude, while that for tics and stereotypies would take on patterns of voluntary movements.
[4] In general, research for treatment of hyperkinesia has most recently been focusing on ameliorating symptoms rather than attempting to correct the pathogenesis of the disease.
As therapies are supported by proven effectiveness that can be repeated in multiple studies, they are useful, but the clinician may also consider that the best treatments for patients can only be evaluated on a case-by-case basis.