Radiculopathy
It may be secondary to intervertebral disk herniation (most commonly at C7 and then the C6 level), degenerative disc disease, osteoarthritis, facet joint degeneration/hypertrophy, ligamentous hypertrophy, spondylolisthesis, or a combination of these factors.
[3][verification needed] Repeated, longer term exposure (5 years or more) to certain work-related activities may put people at risk of developing lumbosacral radiculopathy.
[medical citation needed] Signs and Symptoms Radiculopathy is a diagnosis commonly made by physicians in primary care specialties, orthopedics, physiatry, and neurology.
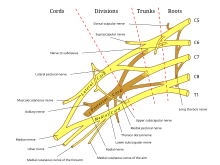
The diagnosis may be suggested by symptoms of pain, numbness, paresthesia, and weakness in a pattern consistent with the distribution of a particular nerve root, such as sciatica.
[medical citation needed] Physical examination may reveal motor and sensory deficits in the distribution of a nerve root.
[3] Shingles is more common among the elderly and immunocompromised; usually (but not always) pain is followed by appearance of a rash with small blisters along a single dermatome.
Cauda equina syndrome should be investigated in case of saddle anesthesia, loss of bladder or bowel control, or leg weakness.
Magnetic resonance imaging (MRI) of the portion of the spine where radiculopathy is suspected may reveal evidence of degenerative change, arthritic disease, or another explanatory lesion responsible for the patient's symptoms.
Needle EMG is the more sensitive portion of the test, and may reveal active denervation in the distribution of the involved nerve root, and neurogenic-appearing voluntary motor units in more chronic radiculopathies.
[14][15] The American Association of Neuromuscular & Electrodiagnostic Medicine has also participated in the Choosing Wisely Campaign and several of their recommendations relate to what tests are unnecessary for neck and back pain.
[16] Ideally, effective treatment aims to resolve the underlying cause and restores the nerve root to normal function.
Conservative treatment may include bed rest, physical therapy, or simply continuing to do usual activities; for pain, nonsteroidal anti-inflammatory drugs, nonopioid or, in some cases, narcotic analgesics may be prescribed.
[17] Evidence also supports consideration of epidural steroid injection with local anesthetic in improving both pain and function in cases of lumbosacral radiculopathy.
Subsequently, a strengthening exercise program should be designed to restore the deconditioned cervical, shoulder girdle, and upper trunk musculature.
[medical citation needed] This is a preferred method of exercise during the sub-acute phase because it resists atrophy and is least likely to exacerbate the condition.
[23] Patients with large cervical disk bulges may be recommended for surgery; however, most often, conservative management will help the herniation regress naturally.