Hypertrophic cardiomyopathy
[3] Specifically, within the bundle branches that conduct impulses through the interventricular septum and into the Purkinje fibers, as these are responsible for the depolarization of contractile cells of both ventricles.
[17] The symptoms of HCM include shortness of breath due to stiffening and decreased blood filling of the ventricles, exertional chest pain (sometimes known as angina) due to reduced blood flow to the coronary arteries, uncomfortable awareness of the heart beat (palpitations), as well as disruption of the electrical system running through the abnormal heart muscle, lightheadedness, weakness, fainting and sudden cardiac death.
[25] Familial hypertrophic cardiomyopathy is inherited as an autosomal dominant trait which is attributed to mutations in one of a number of genes that encode for the sarcomere proteins, and most diagnosed individuals will have an affected parent.
This pulling is thought to occur by several proposed mechanisms, including that flow of blood through the narrowed outflow tract results in it having a higher velocity, and less pressure through the Venturi effect.
In normal individuals, during ventricular systole, the pressure in the ascending aorta and the left ventricle will equalize, and the aortic valve is open.
[citation needed] While the Brockenbrough–Braunwald–Morrow sign is most dramatically demonstrated using simultaneous intra-cardiac and intra-aortic catheters, it can be seen on routine physical examination as a decrease in the pulse pressure in the post-PVC beat in individuals with HCM.
[citation needed] Although HCM may be asymptomatic, affected individuals may present with symptoms ranging from mild to critical heart failure and sudden cardiac death at any point from early childhood to seniority.
[17][42] HCM is the leading cause of sudden cardiac death in young athletes in the United States, and the most common genetic cardiovascular disorder.
Cardiac magnetic resonance imaging (CMR), considered the gold standard for determining the physical properties of the left ventricular wall, can serve as an alternative screening tool when an echocardiogram provides inconclusive results.
[17] Researchers, however, have studied asymptomatic carriers of an HCM-causing mutation through the use of CMR and have been able to identify crypts in the interventricular septal tissue in these people.
It has been proposed that the formation of these crypts is an indication of myocyte disarray and altered vessel walls that may later result in the clinical expression of HCM.
[51] Lastly, genetic testing would provide a definitive diagnosis; however, due to the numerous HCM-causing mutations, this method of screening is complex and is not cost-effective.
This ensures that the test is not wasted on detecting other causes of ventricular hypertrophy (due to its low sensitivity), and that family members of the individual are educated on the potential risk of being carriers of the mutant gene(s).
In people with resting or inducible outflow obstructions, situations that will cause dehydration or vasodilation (such as the use of vasodilatory or diuretic blood pressure medications) should be avoided.
[19] Intravenous phenylephrine (or another pure vasoconstricting agent) can be used in the acute setting of low blood pressure in those with obstructive hypertrophic cardiomyopathy who do not respond to fluid administration.
[7] Cardiac myosin inhibitors reduce left ventricular contractility by decreasing the number of active actin–myosin cross-bridges within the myocyte sarcomere.
[53] Mavacamten was shown to reduce left ventricular outflow tract gradient (a measure of obstruction) and improve symptoms in patients with obstructive hypertrophic cardiomyopathy, and was approved for medical use in the United States in April 2022[54] Aficamten, which has a shorter half life compared with mavacamten, achieves steady state within 2 weeks, and appears to have a wide therapeutic window, was shown to improve peak oxygen uptake during cardiopulmonary exercise testing in patients with New York Heart Association (NYHA) functional class II or III heart failure and decreased exercise capacity.
[42] It involves a median sternotomy (general anesthesia, opening the chest, and cardiopulmonary bypass) and removing a portion of the interventricular septum.
[17][60] When performed properly, an alcohol septal ablation induces a controlled heart attack, in which the portion of the interventricular septum that involves the left ventricular outflow tract is infarcted and will contract into a scar.
This form of treatment has been shown to provide less relief of symptoms and less of a reduction in the left ventricular outflow tract gradient when compared to surgical myectomy.
Although the dual-chamber pacemaker has shown to decrease ventricular outflow tract obstruction, experimental trials have found only a few individuals with improved symptoms.
[42] For people with HCM who exhibit one or more of the major risk factors for sudden cardiac death, an implantable cardioverter-defibrillator (ICD) or a combination pacemaker/ICD all-in-one unit may be recommended as an appropriate precaution.
[68] Nonetheless, recent studies in pediatric cardiology have revealed that HCM accounts for 42% of childhood cardiomyopathies, with an annual incidence rate of 0.47/100,000 in children.
Consequently, the recommended practice is to screen children of affected individuals throughout childhood to detect cardiac abnormalities at an early stage, in the hope of preventing further complications of the disease.
[68] Generally, the diagnosis of HCM in a pediatric population is made during assessment for murmur, congestive heart failure, physical exhaustion, and genetic testing of children of affected individuals.
[76] The first genetic mutation (in cardiac myosin binding protein C) responsible for feline HCM was discovered in 2005 in Maine Coon cats.
Some Maine Coon cats with clinical evidence of hypertrophic cardiomyopathy test negative for this mutation, strongly suggesting that another cause exists in the breed.
[citation needed] Clinically, cats with hypertrophic cardiomyopathy commonly have a systolic anterior motion (SAM) of the mitral valve (see graphic).
They may also develop a left atrial thrombus that embolizes, most commonly, to the terminal aorta creating acute pain and rear limb paralysis (see below).
The FATCAT study at Purdue University demonstrated that it is superior to aspirin for the prevention of a second thrombus from forming in cats that have already experienced a clot.

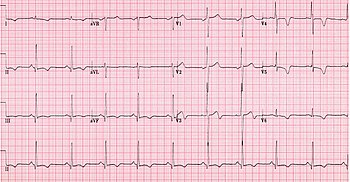

AO = Descending aorta; LV = Left ventricle; ECG = Electrocardiogram.
After the third QRS complex , the ventricle has more time to fill. Since there is more time to fill, the left ventricle will have more volume at the end of diastole (increased preload ). Due to the Frank–Starling law of the heart , the contraction of the left ventricle (and pressure generated by the left ventricle) will be greater on the subsequent beat (beat #4 in this picture). Because of the dynamic nature of the outflow obstruction in HCM, the obstruction increases more than the left ventricular pressure increase. This causes a fall in the aortic pressure as the left ventricular pressure rises (seen as the yellow shaded area in the picture).

