Colposcopy
[1] The main goal of colposcopy is to prevent cervical cancer by detecting and treating precancerous lesions early.
Other reasons for a patient to have a colposcopy include assessment of diethylstilbestrol (DES) exposure in utero, immunosuppression, abnormal appearance of the cervix or as a part of a sexual assault forensic examination.
[9] Colposcopy is not generally performed for people with pap test results showing low-grade squamous intraepithelial lesion (LSIL) or less.
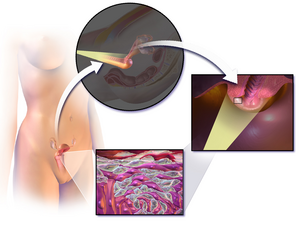
It functions as a lighted binocular or monocular microscope to magnify the view of the cervix, vagina, and vulvar surface.
High magnification together with green filter is often used to identify certain vascular patterns that may indicate the presence of more advanced pre-cancerous or cancerous lesions.
[citation needed] The squamocolumnar junction, or "transformation zone", is a critical area on the cervix where many precancerous and cancerous lesions most often arise.
The ability to see the transformation zone and the entire extent of any lesion visualized determines whether an adequate colposcopic examination is attainable.
[citation needed] Acetic acid solution is applied to the surface of the cervix using cotton swabs to improve visualization of abnormal areas.
Areas of the cervix that turn white (acetowhiteness) after the application of acetic acid or have an abnormal vascular pattern are often considered for biopsy.
[14] Significant complications from a colposcopy are not common but may include bleeding, infection at the biopsy site or endometrium, and failure to identify the lesion.


Type 1: Completely ectocervical (common under hormonal influence).
Type 2: Endocervical component but fully visible (common before puberty).
Type 3: Endocervical component, not fully visible (common after menopause).
