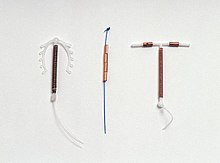
Copper IUD
[16] Because it does not contain hormones, the copper IUD does not disrupt the timing of an individual's menstrual cycle, nor does it prevent ovulation.
[20] An additional advantage of using the copper IUD for emergency contraception is that it can then be used as a form of birth control for 10–12 years after insertion.
[24][25] In the postpartum period, expulsion is less likely when the device is placed less than ten minutes after the placenta is delivered, or when inserted after a cesarean delivery.
If an IUD with copper is inserted after an expulsion has occurred, the risk of re-expulsion has been estimated in one study to be approximately one third of cases after one year.
[11][21][31] The increase in menstrual blood volume varies in different studies but is reported to be as low as 20% and as high as 55%; however, there is no evidence for a concomitant change in ferritin, hemoglobin, or hematocrit.
[33][11][1] If a pregnancy continues with the IUD in place, there is an increased risk of complications including preterm delivery, chorioamnionitis, and spontaneous abortion.
Category 3 contraindications include untreated HIV/AIDS, recent and recurrent exposure to gonorrhea or chlamydia without adequate treatment, benign gestational trophoblastic disease, and ovarian cancer.
[37][38] A copper IUD can be inserted at any phase of the menstrual cycle, as long as pregnancy can be reliably excluded.
It may be inserted in the immediate postpartum period (shortly after delivery of the placenta), and after an induced medical, surgical, or spontaneous abortion provided a genital tract infection can be reliably excluded.
[11][21][16][50] Spermatozoa entering the uterine cavity and cervical mucus are consumed by local phagocytes, and are also directly killed by copper ions and lysosome contents.
[54][55] However, if implantation occurs, there is no evidence that copper affects subsequent development of a pregnancy or causes embryonic failure.
As of 2020[update], IUDs were the most popular method of contraception in fourteen countries, mostly in Central and East Asia.
[56] In Europe, as of 2006[update], copper IUD prevalence ranged from under 5% in the United Kingdom, Germany, and Austria to over 10% in Denmark and the Baltic States.
A similar design was reported by Karl Pust, who wound the free ends of the suture tightly and attached them to a glass disc, which covered the external os.
It was widely used in the UK and the Commonwealth, but discouraged from use in the US and Europe due to the perceived risk of infection, cancer, and inefficacy.
[59][58] In 1934, Japanese physician Tenrei Ōta developed a variation of Gräfenberg's ring that contained a supportive structure in the center.
Though his research was hampered by the fascist government's stance against contraception and his need to spend time in hiding, after World War II he returned to the development of IUDs.
Gold and silver, which had been used by Gräfenberg, were in very short supply in post-war Japan, which led Ōta to other metals, silk, and nylon.
By the end of the 1950s, there were 32 different frame shapes used in Japan, and larger studies showed no connection between these devices and development of endometrial cancer, which had been a theoretical concern due to the inflammatory properties of metals in the uterus.
[60][58] The first plastic device was developed by Lazar Margulies and first trialed in 1959; it was made of a polyethylene ring filled with a radiopaque solution.
Due to its size (6 mm), the cervix had to be dilated prior to insertion, it was poorly tolerated, and the device was prone to expulsion.
[61] Stainless steel was introduced as an alternative to the copper-nickel-zinc alloy in the 1960s and 70s,[58] and was subsequently widely used in China because of low manufacturing costs.
The Chinese government banned production of steel IUDs in 1993 due to high failure rates (up to 10% per year).
[15][62] American obstetrician Howard Tatum conceived the plastic T-shaped IUD in 1967,[63] but its high failure rate (approximately 18%) made it nonviable.
These devices had higher surface areas of copper, and for the first time consistently achieved effectiveness rates of greater than 99%.
The failure rate (in a small number of studies) is very low, 0.1%.34,35 This method definitely prevents implantation, but it is not suitable for women who are not candidates for intrauterine contraception, e.g., multiple sexual partners or a rape victim.