Immunosuppressive drug
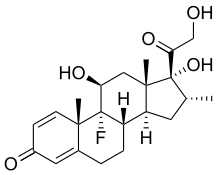
Immunosuppressive drugs can be classified into five groups:[citation needed] In pharmacologic (supraphysiologic) doses, glucocorticoids, such as prednisone, dexamethasone, and hydrocortisone are used to suppress various allergic, inflammatory, and autoimmune disorders.
They act by inhibiting gene expression of cytokines including Interleukin 1 (IL-1), IL-2, IL-3, IL-4, IL-5, IL-6, IL-8, and TNF-alpha by binding to corticosteroid response elements on DNA.
They induce the lipocortin-1 (annexin-1) synthesis, which then binds to cell membranes preventing the phospholipase A2 from coming into contact with its substrate arachidonic acid.
Glucocorticoids also stimulate the lipocortin-1 escaping to the extracellular space, where it binds to the leukocyte membrane receptors and inhibits various inflammatory events: epithelial adhesion, emigration, chemotaxis, phagocytosis, respiratory burst, and the release of various inflammatory mediators (lysosomal enzymes, cytokines, tissue plasminogen activator, chemokines, etc.)
In small doses, it is very efficient in the therapy of systemic lupus erythematosus, autoimmune hemolytic anemias, granulomatosis with polyangiitis, and other immune diseases.
Antibodies are sometimes used as a quick and potent immunosuppressive therapy to prevent the acute rejection reactions as well as a targeted treatment of lymphoproliferative or autoimmune disorders (e.g., anti-CD20 monoclonals).
Heterologous polyclonal antibodies are obtained from the serum of animals (e.g., rabbit, horse), and injected with the patient's thymocytes or lymphocytes.
Polyclonal antibodies inhibit T lymphocytes and cause their lysis, which is both complement-mediated cytolysis and cell-mediated opsonization followed by removal of reticuloendothelial cells from the circulation in the spleen and liver.
Polyclonal antibodies affect all lymphocytes and cause general immunosuppression, possibly leading to post-transplant lymphoproliferative disorders (PTLD) or serious infections, especially by cytomegalovirus.
Patients stay in the hospital as long as three weeks to give the immune system time to recover to a point where there is no longer a risk of serum sickness.
It is possible to diminish their toxicity by using highly purified serum fractions and intravenous administration in the combination with other immunosuppressants, for example, calcineurin inhibitors, cytostatics, and corticosteroids.
The most frequent combination is to use antibodies and ciclosporin simultaneously in order to prevent patients from gradually developing a strong immune response to these drugs, reducing or eliminating their effectiveness.
As such it was one of the first potent immunosuppressive substances and was administered to control the steroid- and/or polyclonal antibodies-resistant acute rejection episodes.
Past this period CD3 blocks the TCR-antigen binding and causes conformational change or the removal of the entire TCR3/CD3 complex from the T-cell surface.
[6] Interleukin-2 is an important immune system regulator necessary for the clone expansion and survival of activated lymphocytes T. Its effects are mediated by the trimer cell surface receptor IL-2a, consisting of the α, β, and γ chains.
Therefore, it is of special significance to the selective immunosuppressive treatment, and research has been focused on the development of effective and safe anti-IL-2 antibodies.
These drugs act by binding the IL-2a receptor's α chain, preventing the IL-2 induced clonal expansion of activated lymphocytes and shortening their survival.
They are used in the prophylaxis of the acute organ rejection after bilateral kidney transplantation, both being similarly effective and with only few side-effects.
The drug also inhibits lymphokine production and interleukin release, leading to a reduced function of effector T-cells.
Ciclosporin is used in the treatment of acute rejection reactions, but has been increasingly substituted with newer, and less nephrotoxic,[7] immunosuppressants.
Calcineurin inhibitors and azathioprine have been linked with post-transplant malignancies and skin cancers in organ transplant recipients.
Non-melanoma skin cancer (NMSC) after kidney transplantation is common and can result in significant morbidity and mortality.
The results of several studies suggest that calcineurin inhibitors have oncogenic properties mainly linked to the production of cytokines that promote tumor growth, metastasis and angiogenesis.
[8] Tacrolimus (trade names Prograf, Astagraf XL, Envarsus XR) is a product of the bacterium Streptomyces tsukubensis.
Sirolimus (rapamycin, trade name Rapamune) is a macrolide lactone, produced by the actinomycete bacterium Streptomyces hygroscopicus.
Infliximab and adalimumab have label warnings stating that patients should be evaluated for latent TB infection and treatment should be initiated prior to starting therapy with them.
Mycophenolic acid acts as a non-competitive, selective, and reversible inhibitor of inosine-5′-monophosphate dehydrogenase (IMPDH), which is a key enzyme in the de novo guanosine nucleotide synthesis.
Actual or suspected immunosuppressive agents can be evaluated in terms of their effects on lymphocyte subpopulations in tissues using immunohistochemistry.