Influenza pandemic
[citation needed] The World Health Organization (WHO) has produced a six-stage classification that describes the process by which a novel influenza virus moves from the first few infections in humans through to a pandemic.
It was thought to be caused by comets, earthquakes, volcanoes, cosmic dust, the rising and setting of the sun, vapors arising from the air and ground, or a blast from the stars.
In humans, common symptoms of influenza infection are fever, sore throat, muscle pains, severe headache, coughing, and weakness and fatigue.
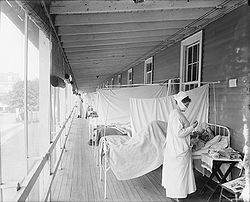
[13] (During the 1918 Spanish flu pandemic, this practice served to promote the evolution of more virulent viral strains over those that produced mild illness.)
When it first killed humans in Asia in the 1990s, a deadly avian strain of H5N1 posed a great risk for a new influenza pandemic; however, this virus did not mutate to spread easily between people.
[66] It was not until the virus had reached Hong Kong in April, however, that the world was alerted to the unusual situation, when the international press began to report on the outbreak.
[67] The World Health Organization was officially informed when the virus arrived in Singapore, which operated the only influenza surveillance laboratory in Southeast Asia,[68] in early May.
[69] From that point on, as the virus continued to sweep the region, the WHO remained attuned to the developing outbreak and helped coordinate the global response for the duration of the pandemic.
[74] Chinese researchers had already come to a similar conclusion in March,[74] but as China was not a member of the WHO nor a part of its network of National Influenza Centers, this information did not reach the rest of the world, a fact which the WHO would lament after the pandemic.
[74] Around this time, extensive epidemics developed in the Northern Hemisphere following the opening of schools, generally peaking in North America and Europe in October.
[74][75] Influenza activity had largely subsided by the end of the year and remained apparently low during the first months of 1958, though some countries, such as the United States, experienced another rise in mortality from respiratory disease, of unclear origin.
[95][93][96] Genetic analysis and several unusual characteristics of the pandemic have prompted speculation that the virus was released to the public through a laboratory accident.
[104] On 1 November 2009, a worldwide update by the WHO stated that "199 countries and overseas territories/communities have officially reported a total of over 482,300 laboratory confirmed cases of the influenza pandemic H1N1 infection, that included 6,071 deaths.
By 26 April the variant had spread widely; with cases reported in Canada, the US, New Zealand, the UK, France, Spain and Israel.
[117] A 13 November 2009 worldwide update by the WHO states that "206 countries and overseas territories/communities have officially reported over 503,536 laboratory confirmed cases of the influenza pandemic H1N1 infection, including 6,250 deaths.
"[129] In 2014, the United States Centers for Disease Control and Prevention (CDC) introduced the Pandemic Intervals Framework for assessing influenza outbreaks.
Longer-term strategies proposed for regions where highly pathogenic H5N1 is endemic in wild birds have included: The main ways available to tackle a flu pandemic initially are behavioural.
[134] The Institute of Medicine has published a number of reports and summaries of workshops on public policy issues related to influenza pandemics.
They are collected in Pandemic Influenza: A Guide to Recent Institute of Medicine Studies and Workshops,[140] and some strategies from these reports are included in the list above.
Due to the high rate of side effects and risk of antiviral resistance, use of adamantanes to fight influenza is limited.
For example, Canadian health authorities say that they are developing the capacity to produce 32 million doses within four months, enough vaccine to inoculate every person in the country.
[154] However, in September 2009, Australia, Brazil, France, Italy, New Zealand, Norway, Switzerland, the UK, and the USA agreed to make 10 percent of their H1N1 vaccine supply available to less-developed countries.
[159] According to The New York Times as of March 2006, "governments worldwide have spent billions planning for a potential influenza pandemic: buying medicines, running disaster drills, [and] developing strategies for tighter border controls" due to the H5N1 threat.
The United States and these international partners have led global efforts to encourage countries to heighten surveillance for outbreaks in poultry and significant numbers of deaths in migratory birds and to rapidly introduce containment measures.
[161] Ongoing detailed mutually coordinated onsite surveillance and analysis of human and animal H5N1 avian flu outbreaks are being conducted and reported by the USGS National Wildlife Health Center, the CDC, the ECDC, the World Health Organization, the European Commission, the National Influenza Centers, and others.
[162][failed verification] In September 2005, David Nabarro, a lead UN health official, warned that a bird flu outbreak could happen at any time and had the potential to kill 5–150 million people.
[164] "[E]fforts by the federal government to prepare for pandemic influenza at the national level include a $100 million DHHS initiative in 2003 to build U.S. vaccine production.
In a speech before the United Nations General Assembly on 14 September 2005, President George W. Bush announced the creation of the International Partnership on Avian and Pandemic Influenza.
The Partnership brings together nations and international organizations to improve global readiness by: On 5 October 2005, Democratic Senators Harry Reid, Evan Bayh, Dick Durbin, Ted Kennedy, Barack Obama, and Tom Harkin introduced the Pandemic Preparedness and Response Act as a proposal to deal with a possible outbreak.
This document was created to address the growing concern over the hazards faced by public health officials when exposed to sick or dying patients.