Klebsiella pneumoniae
Although found in the normal flora of the mouth, skin, and intestines,[1] it can cause destructive changes to human and animal lungs if aspirated, specifically to the alveoli, resulting in bloody, brownish or yellow colored jelly-like sputum.
[citation needed] It is also known as Friedlander's bacillum in honor of Carl Friedländer, a German pathologist, who proposed that this bacterium was the etiological factor for the pneumonia seen especially in immunocompromised individuals such as people with chronic diseases or alcoholics.
Research conducted at King's College, London has implicated molecular mimicry between HLA-B27 and two Klebsiella surface molecules as the cause of ankylosing spondylitis.
[7] The most common condition caused by Klebsiella bacteria outside the hospital is pneumonia, typically in the form of bronchopneumonia and also bronchitis.
[8] It is typically due to aspiration and alcoholism may be a risk factor, though it is also commonly implicated in hospital-acquired urinary tract infections, and COPD (chronic obstructive pulmonary disease) individuals.
[11][12] Individuals with Klebsiella pneumoniae tend to cough up a characteristic sputum, as well as having fever, nausea, tachycardia, and vomiting.
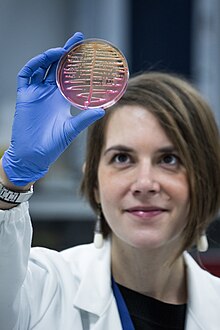
[9] In terms of the diagnosis of Klebsiella pneumoniae the following can be done to determine if the individual has this infection, with the addition of susceptibility testing to identify drug-resistant organisms:[11][9] Treatment for Klebsiella pneumoniae is by antibiotics such as aminoglycosides, piperacillin/tazobactam, and cephalosporins, the choice depending upon antibiotic susceptibility testing, the person's health condition, medical history and severity of the disease.
The bacteria remain susceptible to aminoglycosides and some cephalosporins, and varying degrees of inhibition of the beta-lactamase with clavulanic acid have been reported.
[11][14][15][16] In 2009, strains of K. pneumoniae with gene called New Delhi metallo-beta-lactamase ( NDM-1) that even gives resistance against intravenous antibiotic carbapenem, were discovered in India and Pakistan.
Klebsiella cases in Taiwan have shown abnormal toxicity, causing liver abscesses in people with diabetes mellitus (DM); treatment consists of third generation cephalosporins.
The genetic traits that lead to this pathotype are included in a large virulence plasmid and potentially on additional conjugative elements.
It often spreads to central nervous system and eye causing endophthalmitis, nonhepatic abscesses, pneumonia, necrotizing fasciitis, and meningitis.
[25] Klebsiella species with the ability to produce extended-spectrum beta-lactamases (ESBL) are resistant to virtually all beta-lactam antibiotics, except carbapenems.
Over the past 10 years, a progressive increase in CRKP has been seen worldwide; however, this new emerging nosocomial pathogen is probably best known for an outbreak in Israel that began around 2006 within the healthcare system there.
CRE can be difficult to detect because some strains that harbor blakpc have minimum inhibitory concentrations that are elevated, but still within the susceptible range for carbapenems.
The intervention entailed physical separation of all CRE carriers and appointment of a task force to oversee efficacy of isolation by closely monitoring hospitals and intervening when necessary.
In mid-August 2016, a resident of Washoe County was hospitalized in Reno due to a CRE (specifically Klebsiella pneumoniae) infection.
[citation needed] The table shows the number of AMR genes and plasmids (per strain or subspecies) compared to other common bacteria species.
Alcohol based hand rubs are effective against these Gram-negative bacilli)[43] and wearing gowns and gloves when they enter rooms where patients with Klebsiella-related illnesses are housed.
For urinary tract infections with multidrug-resistant Klebsiella species, a combination therapy with amikacin and meropenem has been suggested.
[44] Multiple drug-resistant K. pneumoniae strains have been killed in vivo by intraperitoneal, intravenous, or intranasal administration of phages in laboratory tests.
[46] New data sources outlining the global burden of K. pneumoniae and drug-resistant forms are expected to build momentum into prophylactic vaccine development.
[47] The recent 2022 IHME study showed that in 2019 K. pneumoniae was responsible for 790,000 deaths [571,000–1,060,000] in all age groups across 11 infectious syndromes.