Leptospirosis
[5] Weil's disease (/ˈvaɪlz/ VILES),[12] the acute, severe form of leptospirosis, causes the infected individual to become jaundiced (skin and eyes become yellow), develop kidney failure, and bleed.
[8] In developing countries, the disease occurs most commonly in pest control, farmers and low-income people who live in areas with poor sanitation.
[5] In developed countries, it occurs during heavy downpours and is a risk to pest controllers, sewage workers[14] and those involved in outdoor activities in warm and wet areas.
The disease begins suddenly with fever accompanied by chills, intense headache, severe muscle aches and abdominal pain.
[5][21] A headache brought on by leptospirosis causes throbbing pain and is characteristically located at the head's bilateral temporal or frontal regions.
[7] The classic form of severe leptospirosis, known as Weil's disease, is characterised by liver damage (causing jaundice), kidney failure, and bleeding, which happens in 5–10% of those infected.
A variety of neurological problems such as paralysis of half of the body, complete inflammation of a whole horizontal section of spinal cord, and Guillain-Barré syndrome are the complications.
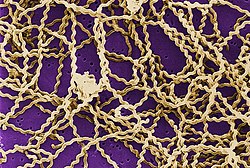
[8] Leptospirosis is caused by spirochaete bacteria that belong to the genus Leptospira, which are aerobic,[8] right-handed helical,[13] and 6–20 micrometers long.
[27] The 19 members of the P1 subclade include the 8 species that can cause severe disease in humans: L. alexanderi, L. borgpetersenii, L. interrogans, L. kirschneri, L. mayottensis, L. noguchii, L. santarosai, and L. weilii.
[21][16] Rats, mice, and moles are important primary hosts, but other mammals including dogs, deer, rabbits, hedgehogs, cows, sheep, swine, raccoons, opossums, and skunks can also carry the disease.
[16] In Africa, a number of wildlife hosts have been identified as carriers, including the banded mongoose, Egyptian fox, Rusa deer, and shrews.
[7] The bacteria enter through cuts, abrasions,[7] ingestion of contaminated food, or contact with mucous membrane of the body (e.g. mouth, nose, and eyes).
[24] Those who have a high risk of sepsis during a leptospirosis infection are found to have the HLA-DQ6 genotype, possibly due to superantigen activation, which damages bodily organs.
In the bloodstream, it can activate host plasminogen to become plasmin that breaks down extracellular matrix, degrades fibrin clots and complemental proteins (C3b and C5) to avoid opsonisation.
[8] Because the bacteria settle in the kidneys, urine cultures will be positive for leptospirosis starting after the second week of illness until 30 days of infection.
If infected, cerebrospinal fluid (CSF) examination shows lymphocytic predominance with a cell count of about 500/mm3, protein between 50 and 100 mg/mL and normal glucose levels.
[25] Leptospiral DNA can be amplified by using polymerase chain reaction (PCR) from serum, urine, aqueous humour, CSF, and autopsy specimens.
[21] Proper use of personal protective equipment (PPE) by people who have a high risk of occupational exposure can prevent leptospirosis infections in most cases.
[16] Doxycycline is given once a week as a prophylaxis and is effective in reducing the rate of leptospirosis infections amongst high-risk individuals in flood-prone areas.
[21] For mild leptospirosis, antibiotic recommendations such as doxycycline, azithromycin, ampicillin, and amoxicillin were based solely on in vitro testing.
When acute kidney failure occurs, early initiation of haemodialysis or peritoneal dialysis can help to improve survival.
[21] Other factors that increase the risk of death include reduced urine output, age more than 36 years, and respiratory failure.
[8] Thirty percent of people with acute leptospirosis complained of long-lasting symptoms characterised by weakness, muscle pain, and headaches.
[28] In anterior uveitis, only topical steroids and mydriatics (an agent that causes dilation of the pupil) are needed while in panuveitis, it requires periocular corticosteroids.
[51] Leptospiral uveitis is characterised by hypopyon, rapidly maturing cataract, free floating vitreous membranes, disc hyperemia and retinal vasculitis.
[63] Leptospira was first observed in 1907 in a post mortem kidney tissue slice by Arthur Stimson using silver deposition staining technique.
[59][64] In 1908, a Japanese research group led by Ryukichi Inada and Yutaka Ito first identified this bacterium as the causative agent of leptospirosis[65] and noted its presence in rats in 1916.
[28] In dogs, the acute clinical signs include fever, loss of appetite, shivering, muscle pain, weakness, and urinary symptoms.
[16] Equine recurrent uveitis (ERU) is the most common disease associated with Leptospira infection in horses in North America and may lead to blindness.
The bacteria can be detected in blood, urine, and milk or liver, kidney, or other tissue samples by using immunofluorescence or immunohistochemical or polymerase chain reaction techniques.