Leukodystrophy
The leukodystrophies are caused by imperfect growth or development of the glial cells which produce the myelin sheath, the fatty insulating covering around nerve fibers.
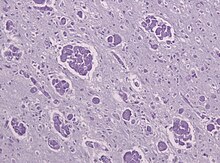
[4] When damage occurs to white matter, subsequent immune responses can lead to inflammation in the central nervous system (CNS), along with the loss of myelin.
Leukodystrophy is characterized by specific symptoms, including decreased motor function, muscle rigidity, and eventual degeneration of sight and hearing.
Treatment options are limited, although hematopoietic stem cell transplantations using bone marrow or cord blood seem to help in certain leukodystrophy types, while further research is being done.
Hyperirritability and hypersensitivity to the environment are common, as well as some tell-tale physical signs including muscle rigidity and a backwards-bent head.
While children do experience optic and auditory degeneration, the course of the disease is usually too rapid, causing death relatively quickly, whereas adults may live with these conditions for many years.
[9] More progressed patients show weakness in deglutition, leading to spastic coughing fits due to inhaled saliva.
[6] While treatments do exist, most are in the experimental phase and can only promise a halt in the progression of symptoms, although some gene therapies have shown some symptomatic improvement.
[11] The debilitating course of the disease has led to numerous philosophical and ethical arguments over experimental clinical trials, patients' rights and physician-assisted suicide.
Each type of leukodystrophy has a unique pathophysiology, but all five of these in some way affect a subset of glial cells, therefore disrupting myelin production and maintenance, and usually involve a mutation involving genes that code for enzymes necessary for the catabolism of very long chain fatty acids (VLCFAs) that are toxic to the myelin-producing cells of the central nervous system.
[16] Metachromatic leukodystrophy is the result of genetic defects in the enzymes associated with the cellular compartment called the lysosome.
[17] This accumulation of sulfatides is toxic to oligodendrocytes, the myelin-producing cells of the CNS, effectively leading to a disturbance in myelin structure followed by demyelination.
[18] Like MLD, Krabbe disease is another type of leukodystrophy with autosomal recessive inheritance that is the result of a lysosomal storage disorder.
It is due to a deletion in exon 16 of the GALC gene that causes a frameshift mutation leading to a premature stop codon.
[19] GALC is a lysosomal enzyme responsible for the catabolism of galactolipids, especially the toxic lipid psychosine, that are widely distributed throughout the brain.
A deficiency in GALC thus causes a buildup of these fatty acids, leading to an incursion by cells called "globoid macrophages" that destroy oligodendrocytes, thereby inhibiting any further myelin formation.
It is speculated that the accumulated and embedded VLCFA in the complex lipids could lead to the destabilization of the myelin sheath and eventually to demyelination.
[citation needed] Alexander disease is unique from the leukodystrophies mentioned above, in that it is the result of spontaneous mutation, meaning that it is not inherited.
[23] Intermediate filaments are proteins responsible for the makeup of the cellular cytoskeleton; thus, this type of mutation causes abnormal structural development of a person's cells.
Stem cell transplants and gene therapy appear to be the most promising in treating all leukodystrophies, providing they take place as early as possible, prior to extensive neurological damage.
[11] Current gene therapy research for metachromatic leukodystrophy has been reviewed with an emphasis on ex vivo transplantation of genetically modified hematopoietic stem cells.
[28][needs update] Currently, no research has shown a higher prevalence of most leukodystrophy types in any one place around the world.
Each year, ELA invites the international scientific community to submit research projects in the field of genetic leukodystrophies, the cerebral white matter in premature infants, and of myelin repair.
[33] The United Leukodystrophy Foundation (ULF), incorporated in 1982, is a non-profit, voluntary health organization dedicated to funding cutting-edge research and to providing patients and their families with disease information and medical referrals.