Lung microbiota
The lung microbiota is the pulmonary microbial community consisting of a complex variety of microorganisms found in the lower respiratory tract particularly on the mucous layer and the epithelial surfaces.
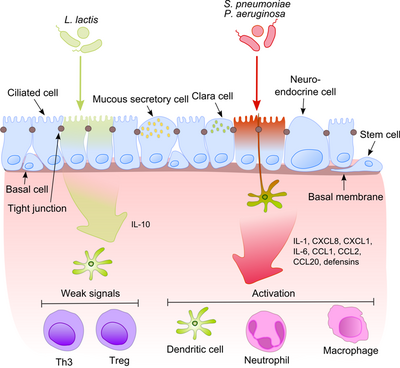
After recognition of pathogenic bacteria proinflammatory pathways are activated and cellular components of the adaptive and innate immunity are recruited to the infection site.
The DNA-binding protein complex recognizes a discrete nucleotide sequence (5’-GGG ACT TTC T-3’) in the upstream region of a variety of response genes.
[8] Another explanation of commensal tolerance of the epithelium refers to the post-translational modification of a protein by the covalent attachment of one or more ubiquitin (Ub) monomers.
The inhibition of ubiquitination leads to reduction of inflammation, because only polyubiquitinated (IκB-κ is targeted for degradation by the 26 S proteasome, allowing NF-κB translocation to the nucleus and activation the transcription of effector genes (for example IL-8).
Probiotic bacteria such as Lactobacilli are able to modulate the activity of the Ub-proteasome system via inducing reactive oxygen species (ROS) production in epithelial cells.
In mammalian cells, ROS have been shown to serve as critical second messengers in multiple signal transduction pathways in response to proinflammatory cytokines.
Bacterially induced ROS causes oxidative inactivation of the catalytic cysteine residue of Ub 12 resulting in incomplete but transient loss of cullin-1 neddylation and consequent effects on NF-κB and β-catenin signaling.
Another commensal species, B. thetaiotaomicron, attenuates pro-inflammatory cytokine expression by promoting nuclear export of NF-κB subunit RelA, through a peroxisome proliferator activated receptor γ (PPAR-γ)-dependent pathway.
On the other hand, Prevotella, Mesorhizobium, Microbacterium, Micrococcus, Veillonela, Rhizobium, Stenotrophomonas, and Lactococcus present mostly in healthy individual cohort.