Medicaid
In the United States, Medicaid is a government program that provides health insurance for adults and children with limited income and resources.
Medicaid was established in 1965, part of the Great Society set of programs during President Lyndon B. Johnson’s Administration, and was significantly expanded by the Affordable Care Act (ACA), which was passed in 2010.
[10] Medicaid covers healthcare costs for people with low incomes, while Medicare is a universal program providing health coverage for the elderly.
Under managed care, Medicaid recipients are enrolled in a private health plan, which receives a fixed monthly premium from the state.
The states pay a monthly capitated rate per member to the MCOs, which in turn provide comprehensive care and accept the risk of managing total costs.
The objective was to help states assist residents whose income and resources were insufficient to pay the costs of traditional commercial health insurance plans.
Before the law was passed, some states did not allow able-bodied adults to participate in Medicaid, and many set income eligibility far below the Federal poverty level.
Under the provisions of the law, any state that participated in Medicaid would need to expand coverage to include anyone earning up to 138% of the Federal poverty level beginning in 2014.
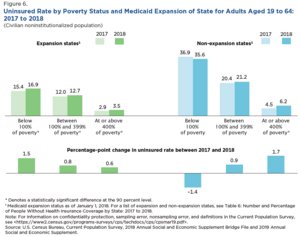
[25][26][27][28] However, in 2012, the Supreme Court held in National Federation of Independent Business v. Sebelius that withdrawing all Medicaid funding from states that refused to expand eligibility was unconstitutionally coercive.
[32] The Kaiser Family Foundation estimated in October 2015 that 3.1 million additional people were not covered in states that rejected the Medicaid expansion.
[38][39] Some studies suggested that rejecting the expansion would cost more due to increased spending on uncompensated emergency care that otherwise would have been partially paid for by Medicaid coverage.
[40] A 2016 study found that residents of Kentucky and Arkansas, which both expanded Medicaid, were more likely to receive health care services and less likely to incur emergency room costs or have trouble paying their medical bills.
[42] A 2016 DHHS study found that states that expanded Medicaid had lower premiums on exchange policies because they had fewer low-income enrollees, whose health, on average, is worse than that of people with higher income.
[24] A July 2019 study by the National Bureau of Economic Research (NBER) indicated that states enacting Medicaid expansion exhibited statistically significant reductions in mortality rates.
A few of those programs are listed below: As of January 2012, Medicaid and/or CHIP funds could be obtained to help pay employer health care premiums in Alabama, Alaska, Arizona, Colorado, Florida, and Georgia.
According to a study conducted by Gideon Lukens, factors significantly affecting eligibility included "party control, the ideology of state citizens, the prevalence of women in legislatures, the line-item veto, and physician interest group size".
In its implementation, this has meant using Medicaid funds to pay for low-income citizens' health insurance; this private-option was originally carried out in Arkansas but was adopted by other Republican-led states.
[53] Certain groups of people, such as migrants, face more barriers to health care than others due to factors besides policy, such as status, transportation and knowledge of the healthcare system (including eligibility).
[84] These other requirements include, but are not limited to, assets, age, pregnancy, disability,[85] blindness, income, and resources, and one's status as a U.S. citizen or a lawfully admitted immigrant.
[87] The Deficit Reduction Act of 2005 (DRA) requires anyone seeking Medicaid to produce documents to prove that he is a United States citizen or resident alien.
Once someone is approved as a beneficiary in the Supplemental Security Income program, they may automatically be eligible for Medicaid coverage (depending on the laws of the state they reside in).
The penalty is determined by dividing the average monthly cost of nursing home care in the area or State into the amount of assets gifted.
All transfers made during the five-year look-back period are totaled, and the applicant is penalized based on that amount after having already dropped below the Medicaid asset limit.
Legal permanent residents (LPRs) with a substantial work history (defined as 40 quarters of Social Security covered earnings) or military connection are eligible for the full range of major federal means-tested benefit programs, including Medicaid (Medi-Cal).
Special rules apply to several limited noncitizen categories: certain "cross-border" American Indians, Hmong/Highland Laotians, parolees and conditional entrants, and cases of abuse.
[112] In 1993, Congress enacted the Omnibus Budget Reconciliation Act of 1993, which required states to attempt to recoup "the expense of long-term care and related costs for deceased Medicaid recipients 55 or older.
"[117] A 2016 paper found that Medicaid has substantial positive long-term effects on the health of recipients: "Early childhood Medicaid eligibility reduces mortality and disability and, for whites, increases extensive margin labor supply, and reduces receipt of disability transfer programs and public health insurance up to 50 years later.
[122] A 2021 study found that expansions of adult Medicaid dental coverage increasingly led dentists to locate to poor, previously underserved areas.
[125][126][127] A 2017 paper found that Medicaid expansion under the Affordable Care Act "reduced unpaid medical bills sent to collection by $3.4 billion in its first two years, prevented new delinquencies, and improved credit scores.
The proposed mechanisms for the reduction were that Medicaid increased the economic security of individuals and provided greater access to treatment for substance abuse or behavioral disorders.