Merkel-cell carcinoma
Merkel cell carcinoma (MCC) is a rare and aggressive skin cancer occurring in about three people per million members of the population.
[2] Factors involved in the development of MCC include the Merkel cell polyomavirus (MCPyV or MCV), a weakened immune system, and exposure to ultraviolet radiation.
[7] Five key attributes of MCC were summarized in 2008 in the acronym AEIOU (Asymptomatic/lack of tenderness, Expanding rapidly, Immune suppression, Older than 50 years, and Ultraviolet-exposed site on a person with fair skin).
[11] Merkel cell cancers tend to invade locally, infiltrating the underlying subcutaneous fat, fascia, and muscle, and typically metastasize early in their natural history, most often to the regional lymph nodes.
[14] Additionally, they have not been shown to support Merkel cell polyoma virus infection, which is believed to drive oncogenesis in approximately 80% of MCC.
Additionally, in vitro experiments have demonstrated that fibroblasts not only support Merkel cell polyomavirus (MCV) infection but can be induced into having a MCC phenotype by the expression of viral proteins.
[19] Several factors are involved in the pathophysiology of MCC, including MCV, ultraviolet radiation (UV) exposure, and weakened immune function.
[23] Normally, patients infected with MCV show low levels of antibodies to the LT protein, perhaps due to a nuclear localization domain in its C-terminal that limits its cellular dispersion.
[24] The N-terminal LXCXE motif of the LT protein has been shown to interact with known oncogene Rb and is conserved in other cancer-causing viruses.
[24] Studies suggest that LT may also preserve cell proliferation signals such as c-Myc and cyclin E and cause DNA injury to the p53 tumor suppressor.
[6][10] The incidence of MCC is increased in conditions with defective immune functions such as malignancy, HIV infection, and organ transplant patients, etc.
[26] The body of data indicating the importance of immune function in MCC pathogenesis has been exploited for the development of immunotherapies discussed below.
Diagnosis of MCC begins with a clinical examination of the skin and lymph nodes to determine suspicious areas for further investigation.
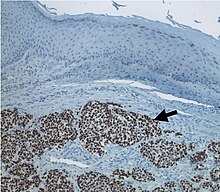
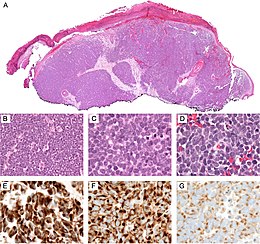
On light microscopy, MCC shows basaloid tumor nests with neuroendocrine features ("salt and pepper" chromatin, scarce cytoplasm, and brisk mitotic activity).
[6][28] In addition to standard examination under light microscopy, immunohistochemistry (IHC) is also generally required to differentiate MCC from other morphologically similar tumors such as skin metastases of small cell lung cancer, the small cell variant of melanoma, various cutaneous leukemic/lymphoid neoplasms, and Ewing's sarcoma.
Once an MCC diagnosis is made, a sentinel lymph node biopsy as well as imaging are recommended as a part of the staging process, which determines prognosis and subsequent treatment options.
The World Health Organization, American Academy of Dermatology, and Skin Cancer Foundation recommend the following measures to prevent excessive UV exposure and skin cancer:[30][31][32] Merkel cell carcinoma is typically treated with surgery and radiation; immunotherapy is used in advanced disease.
The largest studies to date, from Australia, demonstrated that radiotherapy alone achieves equal outcomes with upfront or neoadjuvant surgery followed by radiation therapy.
There have been no head-to-head trials comparing the two treatment strategies, and in the absence of this, surgeons tend to most commonly perform excisional biopsy prior to referring for radiation therapy to eradicate MCC.
[25] The most recent American guidelines do not recommend adjuvant chemotherapy, citing a lack of evidence to suggest improved outcomes.
[40] Due to their side effects, however, National Comprehensive Cancer Network guidelines recommend PD-1 inhibitors for people with disseminated rather than early-stage MCC.
[23][24][25][37] According to the American Joint Committee on Cancer (AJCC), the natural course of MCC is "variable and depends heavily on the stage at diagnosis".
[58] Since 2006, it has been known that other primary cancers increase the risk of MCC significantly, especially in those with the prior multiple myeloma, chronic lymphocytic leukemia, and malignant melanoma.
[20] Friedrich Sigmund Merkel (1845–1919) was a German anatomist and histopathologist who first described the Tastzellen (touch cells) in the skin in 1875.