Merkel cell polyomavirus
[1] It was the first example of a human viral pathogen discovered using unbiased metagenomic next-generation sequencing with a technique called digital transcriptome subtraction.
It is suspected to cause the majority of cases of Merkel cell carcinoma, a rare but aggressive form of skin cancer.
However, it has also been found elsewhere, such as in shedded healthy skin and gastrointestinal tract tissues, thus its precise mode of transmission remains unknown.
[6][7] In addition, recent studies suggest that this virus may latently infect the human sera[8] and peripheral blood mononuclear cells.
The LT antigen possesses a helicase motif needed for virus replication that is deleted in MCC tumors.
Unlike for other polyomaviruses, MCV sT antigen transforms cells in vitro [16] by activating cap-dependent translation.
Although rare compared with other skin cancers, the incidence of Merkel cell carcinoma in the United States tripled between 1986 and 2001, to around 1400 cases per year.
Kaposi's sarcoma and Burkitt's lymphoma are examples of tumors known to have a viral etiology that occur at increased frequency in immunosuppressed people.
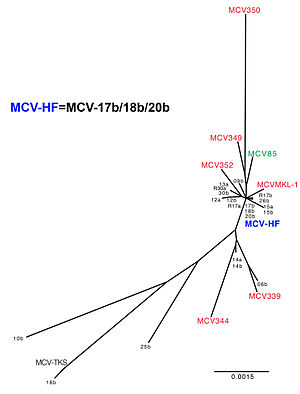
Sequencing of the virus from Merkel cell cancers reveals that it generally has tumor-specific mutations that truncate the MCV T antigen.
Examination of infected tumors reveals that the majority have a clear monoclonal pattern, indicating that the virus integrated into a single cell before it began its cancerous expansion.
Persons with immunosuppression (e.g., AIDS or organ transplant patients) are at higher risk for this cancer and may benefit from periodic skin examinations.
Biopsy of a Merkel cell tumor should readily provide a diagnosis and when caught early, has a good prognosis through standard treatment.
Caution is needed in interpreting results from PCR since it is prone to false-positive contamination and a substantial fraction of healthy skin samples may harbor low-level infection.
[30][31] Blood tests have also been developed[4][5] that show the majority of adults have been previously exposed to MCV and may continue to carry it as an asymptomatic infection.
The importance of this finding is that a promising rational drug target was uncovered within four years of the initial discovery of the virus and that other new treatments might be rapidly developed now that the cause of the cancer is known.
MCV is a target for cell-mediated immune responses, and so important research efforts are being focused on immunologic therapies that may benefit MCC patients.
[citation needed] Yuan Chang and Patrick S. Moore discovered Kaposi's sarcoma-associated herpesvirus by a physical subtraction method in 1994.
When this was performed on four cases of Merkel cell carcinoma, one cDNA was found that was similar to sequences of known polyomaviruses but clearly distinct enough that it could be shown to be a new virus.
This was quickly confirmed by studies of MCC patients from around the world, including evidence for monoclonal integration of the virus in these tumors.
At this time no test for the presence of the virus is generally available, nor would patients be advised to change their treatment based on knowledge of MCV infection status.