Microsporum gypseum
Microsporum gypseum is a soil-associated dermatophyte that occasionally is known to colonise and infect the upper dead layers of the skin of mammals.
[1] The name refers to an asexual "form-taxon" that has been associated with four related biological species of fungi: the pathogenic taxa Arthroderma incurvatum, A. gypsea, A. fulva and the non-pathogenic saprotroph A.
[7] The teleomorphic states of this species were originally the first to be discovered[3] by Arturo Nannizii for M. gypseum in 1927, but his contribution was largely ignored by the scientific community.
[6] Until Christine Dawson and J.C. Gentles discovered anamorph Arthroderma uncurvatum, the teleomorph of Trichophyton ajelloi.
Griffin rediscovered M. gypseum by Nanizzi, and another individual P.M. Stockdale also isolated the second teleomorph of the species naming it Nannizzia incurvatum.
[3] It is now believed that very similar anamorphs, M. gypseum and M. fulvum, consist of three teleomorphs: N. gypsea, N. incurvatum, and N.
[5] The ascoma of the fungus is a globose, appendaged gymnothecium that is pale buff in colour and 500–1250 μm in diameter.
[4] The peridial hyphae are hyaline, pale buff, septate, and are branched with thinly but have densely verrucose walls.
[4] Microconidia are drop shaped, clavate, (1.7–3.5 x 3.3–8.3 μm), unicellular, smooth-walled or can be slightly roughened and are created laterally on the hyphae.
[4] Additionally, the spiral hyphal appendages that ornament the ascomata are often produced spontaneously in culture in the absence of gymnothecia.
[5] Comparatively A. gypseum produces more spreading and a coarser granular colony; the macroconidia also are wider and the surface colour is brighter and redder than A. incurvatum.
Colonies of A. incurvatum are pale buff in colour and finely granular, occasionally with a reddish to yellow reverse.
[9] The species itself commonly infects humans whom are closely tied to these areas because of agricultural work.
[7] The diseases it causes is classified as tinea or ringworm, with an adjective prescribing to the afflicted body part.
[1] Tinea corporis, as well; this is characterized as an intense inflammatory response resembling a bacterial infection, thus surgical intervention is not needed because inflammation is due to the fungus alone.
[4] So as such animals like cattle are commonly affected but horses, rodents, monkeys and dogs have a tendency to acquire it.
[5][8] Microsporum gypseum is categorized as a rare agent of infection, and usually only occurs in rural areas.
[13] The lesions are usually inflammatory, impetiginous, and sometimes bullous with rapid development and resolution; this is accompanied by scarring and permanent patches alopecia.
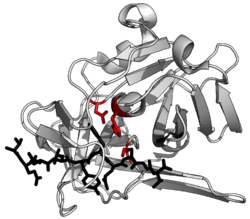
[14] The extracellular proteases released assist the fungus in invading the host skin barrier (keratin rich) with the presence of keratinase (keratinolytic activity increases).
[14] They then use the proteases to enhance their survival by chemically or physically altering the environment to their benefit by digesting the host proteins, thus providing themselves with nutrition.
These proteases are found in all stages of growth (lag to declining) but peak at the mid log phase.
[15] Animal treatment is usually done with itraconazole or ketoconazole; most European countries use off label terbinafine in cats and dogs.
[16] The mistreatment of fungal pathogens is due to the thought of bacterial infection and the administration of corticosteroids.