Myalgic encephalomyelitis/chronic fatigue syndrome
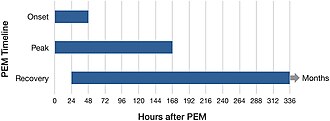
The hallmark symptom is post-exertional malaise, a worsening of the illness which can start immediately or hours to days after even minor physical or mental activity.
[22] ME/CFS has been classified as a neurological disease by the World Health Organization (WHO) since 1969, initially under the name benign myalgic encephalomyelitis.
[11][26] PAISes such as long COVID and post-treatment Lyme disease syndrome share many symptoms with ME/CFS and are suspected to have a similar cause.
[28] A 2015 report from the US Institute of Medicine recommended the illness be renamed systemic exertion intolerance disease (SEID) and suggested new diagnostic criteria.
[30] ME/CFS causes debilitating fatigue, sleep problems, and post-exertional malaise (PEM, overall symptoms getting worse after mild activity).
In addition, cognitive issues, orthostatic intolerance (dizziness or nausea when upright) or other physical symptoms may be present (see also § Diagnostic criteria).
When starting an activity, muscle strength may drop rapidly, which can lead to difficulty with coordination, clumsiness or sudden weakness.
[10]: 6 Extended periods of PEM, commonly referred to as "crashes" or "flare-ups" by people with the illness, can lead to a prolonged relapse.
[3] Some have postural orthostatic tachycardia syndrome (POTS), an excessive increase in heart rate after standing up, which can result in fainting.
[29]: 16 Additional common symptoms include irritable bowel syndrome or other problems with digestion, chills and night sweats, shortness of breath or an irregular heartbeat.
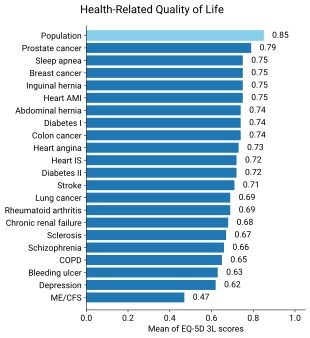
[12] Individuals with ME/CFS have decreased quality of life when evaluated by the SF-36 questionnaire, especially in the domains of physical and social functioning, general health, and vitality.
[9] Viral infections have long been suspected to cause ME/CFS, based on the observation that ME/CFS sometimes occurs in outbreaks and is possibly connected to autoimmune diseases.
Other consistent findings, based on a smaller number of studies, are low metabolism in some areas, reduced serotonin transporters, and problems with neurovascular coupling.
More direct evidence from two small positron emission tomography studies of microglia, a type of immune cell in the brain, were contradictory, however.
On the second test, healthy people's scores stay roughly the same or increase slightly, while those with ME/CFS have a clinically significant decrease in work rate at the anaerobic threshold.
Diagnosis requires fatigue, PEM, non-restorative sleep, and either cognitive issues (such as memory impairment) or orthostatic intolerance.
Additionally, fatigue must persist for at least six months, substantially impair activities in all areas of life, and have a clearly defined onset.
[64] Pacing is difficult to apply for people with very severe ME/CFS, as the activities that trigger PEM in this group, such as eating, cannot be avoided completely.
[12] People with moderate to severe ME/CFS may benefit from home adaptations and mobility aids, such as wheelchairs, disability parking, shower chairs, or stair lifts.
[69] Symptoms of severe ME/CFS may be misunderstood as neglect or abuse during well-being evaluations, and NICE recommends that professionals with experience in ME/CFS should be involved in any type of assessment for safeguarding.
[33] Factors that may make the disease worse over days, but also over longer periods, are physical and mental exertion, a new infection, sleep deprivation, and emotional stress.
[72] In 1970, two UK psychiatrists proposed that these ME outbreaks were psychosocial phenomena, suggesting mass hysteria or altered medical perception as potential causes.
[1]: 28–29 Melvin Ramsay's later research highlighted ME's disabling nature, prompting the removal of "benign" from the name and the creation of diagnostic criteria in 1986.
These criteria included the tendency of muscles to tire after minor effort and take multiple days to recover, high symptom variability, and chronicity.
Despite Ramsay's work and a UK report affirming that ME was not a psychological condition, scepticism persisted within the medical field, leading to limited research.
Following this, the US National Institutes of Health published their Pathways to Prevention report, which gave recommendations on research priorities.
A reanalysis under the original clinical trial protocol showed no significant difference in recovery rate between treatment groups and the controls receiving standard care.
[83] They may also feel forced to prove that they are legitimately ill.[84] Some may be given outdated treatments that provoke symptoms or assume their illness is due to unhelpful thoughts and deconditioning.
[96] Worldwide, multiple sclerosis, which affects fewer people and results in disability no worse than ME/CFS, received 20 times as much funding between 2007 and 2015.
This may explain why COPD, a severe lung disease often caused by smoking, receives low funding per healthy life year lost.