Nerve block
Local anesthetic is often combined with other drugs to potentiate or prolong the analgesia produced by the nerve block.
Regional blocks can be used for procedural anesthesia, post-operative analgesia, and treatment of acute pain in the emergency room.
Imaging such as MRI has poor correlation with clinical diagnosis of nerve entrapment as well as intraoperative findings of decompression surgeries and so diagnostic blocks are used for surgical planning.
[9] Local anesthetic nerve blocks are sterile procedures usually performed in an outpatient facility or hospital.
The procedure can be performed with the help of ultrasound, fluoroscopy, CT, or MRI/MRN to guide the practitioner in the placement of the needle.
Landmark-guided (or "blind") nerve blocks use palpable anatomical landmarks and a working knowledge of the superficial and deep anatomy to determine where to place the needle.
[24] Next hand-operated probe can make the images challenging for surgical planning when the exact needle location must be known.
The limited penetration depth and resolution tends to make ultrasound a poor choice in particular for deeply situated pelvic nerves.
[27] MRI provides excellent visualization of soft tissues, but the detail is not usually enough to see the small nerves that are often entrapped.
Newer technology (MR neurography), however, has increased the level of nerve details seen and allowed for more accurate MRI-directed injections.
MRN-guided blocks are especially effective for deep, small nerves which are otherwise difficult to visualize with ultrasound and CT.
[7] However, due to the expense of MRI machines, MRN-guidance is not a substitute for other imaging modalities but rather a specialized tool which higher accuracy is required.
[29] Drugs commonly used for peripheral nerve blocks include lidocaine, ropivacaine, bupivacaine, and mepivacaine.
[30] Local anesthetics act on the voltage-gated sodium channels that conduct electrical impulses and mediate fast depolarization along nerves.
Lipid solubility, blood flow in the tissue, and presence of vasoconstrictors with the anesthetic all play a role in this.
[29] A higher lipid solubility makes the anesthetic more potent and have a longer duration of action; however, it also increases the toxicity of the drug.
[29] Local anaesthetics are often combined with adjuvants, drugs that boost the effect of each other, with the end goal of increasing the duration of the analgesia or shortening time of onset.
[34] It is unclear if the use of epinephrine in addition to lidocaine is safe for nerve blocks of fingers and toes due to insufficient evidence.
[29] Nerve blocks may also reduce the risk of developing persistent postoperative pain several months after surgery.
[39] Local anesthetic nerve blocks are sterile procedures that can be performed with the help of anatomical landmarks, ultrasound, fluoroscopy (a live X-ray), or CT. Use of any one of these imaging modalities enables the physician to view the placement of the needle.
[10] Local anesthetic toxicity, the most dangerous complication, is often first detected by symptoms of numbness and tingling around the mouth, metallic taste, or ringing in the ears.
Nerve injury most often occurs from ischaemia, compression, direct neurotoxicity, needle laceration, and inflammation.
[45] This surgery is performed in rare cases of severe chronic pain where no other treatments have been successful, and for other conditions such as involuntary twitching and excessive blushing or sweating.
[47] A brief "rehearsal" local anesthetic nerve block is usually performed before the actual neurectomy to determine efficacy and detect side effects.
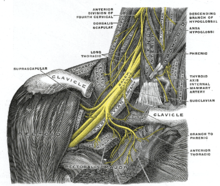
[47] The brachial plexus is a bundle of nerves innervating the shoulder and arm and can be blocked at different levels depending on the type of upper extremity surgery being performed.
[48] The interscalene block is done at the neck where the brachial plexus emerges between the anterior and middle scalene muscles.
[53] The lumbar plexus block is an advanced technique indicated for hip, anterior thigh, and knee surgery.
[61] One of the first instances on using continuous paravertebral blockade in the body was by the thoracic team led by Sabanathan in Bradford.
[63] The paravertebral space is located a couple centimeters lateral to the spinous process and is bounded posteriorly by the superior costotransverse ligament and anteriorly by the parietal pleura.
[63] The erector spinae plan block is sometimes suggested for thoracic-related pain control to reduce the need for opioids after surgery.