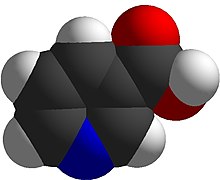
Nicotinic acid
[7] Despite the proven lipid changes, nicotinic acid has not been found useful for decreasing the risk of cardiovascular disease in those already prescribed a statin drug.
[8] A 2010 review had concluded that nicotinic acid was effective as a mono-therapy,[9] but a 2017 review incorporating twice as many trials concluded that prescription nicotinic acid, while affecting lipid levels, did not reduce all-cause mortality, cardiovascular mortality, myocardial infarctions, nor fatal or non-fatal strokes.
[18] The term "nicotinic acid" unambiguously refers to the substance and the prescription medicine containing it, which treats elevated cholesterol and triglycerides.
NAD is important in catabolism of fat, carbohydrate, protein, and alcohol, as well as cell signaling and DNA repair, and NADP mostly in anabolism reactions such as fatty acid and cholesterol synthesis.
[23][20] In the United States, nicotinic acid is sold as a non-prescription dietary supplement with a range of 100 to 1000 mg per serving.
Face, arms and chest skin turns a reddish color because of vasodilation of small subcutaneous blood vessels, accompanied by sensations of heat, tingling and itching.
[4] Prescription nicotinic acid, commonly labeled as niacin in the United States, is available in immediate-release and slow-release formulations.
[29][30] HCA2 and HCA3 inhibit cyclic adenosine monophosphate (cAMP) production and thus suppress the release of free fatty acids (FFAs) from body fat, reducing their availability to the liver to synthesize the blood-circulating lipids in question.
[31][32][33] A decrease in free fatty acids also suppresses liver expression of apolipoprotein C3 and PPARg coactivator-1b, thus increasing VLDL-C turnover and reducing its production.
[34] Nicotinic acid also directly inhibits the action of diacylglycerol O-acyltransferase 2 (DGAT2) a key enzyme for triglyceride synthesis.
Nicotinic acid increases apolipoprotein A1 levels by inhibiting the breakdown of this protein, which is a component of HDL particles.
[35][36] It also inhibits HDL-C hepatic uptake by suppressing production of the cholesterol ester transfer protein (CETP) gene.
The reason given: "Based on the collective evidence from several large cardiovascular outcome trials, the Agency has concluded that the totality of the scientific evidence no longer supports the conclusion that a drug-induced reduction in triglyceride levels and/or increase in HDL-cholesterol levels in statin-treated patients results in a reduction in the risk of cardiovascular events."
[17][43] Both products are contraindicated for people with existing peptic ulcer disease, or other bleeding problems because nicotinic acid lowers platelet count and interferes with blood clotting.
These products are contraindicated for women who are lactating because it is known that nicotinic acid is excreted into human milk, but the amount and potential for adverse effects in the nursing infant are not known.
[19][17][43] The most common adverse effects of medicinal nicotinic acid (500–3000 mg) are flushing (e.g., warmth, redness, itching or tingling) of the face, neck and chest, headache, abdominal pain, diarrhea, dyspepsia, nausea, vomiting, rhinitis, pruritus and rash.
[43] The acute adverse effects of high-dose nicotinic acid therapy (1–3 grams per day) – which is commonly used in the treatment of hyperlipidemias – can further include hypotension, fatigue, glucose intolerance and insulin resistance, heartburn, blurred or impaired vision, and macular edema.
[5][4] With long-term use, the adverse effects of high-dose nicotinic acid therapy (750 mg per day) also include liver failure (associated with fatigue, nausea, and loss of appetite), hepatitis, and acute liver failure;[5][4] these hepatotoxic effects of nicotinic acid occur more often when extended-release dosage forms are used.
[5][4] The long-term use of nicotinic acid at greater than or equal to 2 grams per day also significantly increases the risk of cerebral hemorrhage, ischemic stroke, gastrointestinal ulceration and bleeding, diabetes, dyspepsia, and diarrhea.
[49][50] Nicotinic acid in medicinal doses can cause modest elevations in serum transaminase and unconjugated bilirubin, both biomarkers of liver injury.
Early symptoms of serious liver damage include nausea, vomiting and abdominal pain, followed by jaundice and pruritus.
[11] The high doses of nicotinic acid used to treat hyperlipidemia have been shown to elevate fasting blood glucose in people with type 2 diabetes.
[12][13] High doses of nicotinic acid can also cause niacin maculopathy, a thickening of the macula and retina, which leads to blurred vision and blindness.
[17] Activating HCA2 has effects other than lowering serum cholesterol and triglyceride concentrations: antioxidative, anti-inflammatory, antithrombotic, improved endothelial function and plaque stability, all of which counter development and progression of atherosclerosis.
[57] One test used to aid in diagnosing Gilbert's Syndrome involves intravenous administration of nicotinic acid (niacin) in a dose of 50 mg over a period of 30 seconds.
Unlike some other vitamins, the percent absorbed does not decrease with increasing dose, so that even at amounts of 3-4 grams, absorption is nearly complete.
In 2018, it was discovered that a nicotinic acid factory in Visp, Switzerland, was responsible for around one percent of the country's greenhouse gas emissions.
Niaspan has a film coating that delays release of the nicotinic acid, resulting in an absorption over a period of 8–12 hours.
[75][76] Niacin as a chemical compound was first described by chemist Hugo Weidel in 1873 in his studies of nicotine,[77] but that predated by many years the concept of food components other than protein, fat and carbohydrates that were essential for life.
[86] In the late 1930s, studies by Tom Douglas Spies, Marion Blankenhorn, and Clark Cooper confirmed that nicotinic acid cured pellagra in humans.