Norepinephrine transporter
[5] NET is a monoamine transporter and is responsible for the sodium-chloride (Na+/Cl−)-dependent reuptake of extracellular norepinephrine (NE), which is also known as noradrenaline.
[7] An epigenetic mechanism (hypermethylation of CpG islands in the NET gene promoter region) that results in reduced expression of the noradrenaline (norepinephrine) transporter and consequently a phenotype of impaired neuronal reuptake of norepinephrine has been implicated in both postural orthostatic tachycardia syndrome and panic disorder.
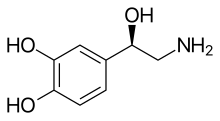
NE, also known as noradrenaline (NA), has an important role in controlling mood, arousal, memory, learning, and pain perception.
[17] Norepinephrine transporters are confined to the neurons of the sympathetic system, and those innervating the adrenal medulla, lung, and placenta.
[19] The amino acid sequence of NET has shown multiple sites related to protein kinase phosphorylation.
[17] Post-translational modifications can have a wide range of effects on the function of the NET, including the rate of fusion of NET-containing vesicles with the plasma membrane, and transporter turnover.
[19] Orthostatic intolerance (OI) is a disorder of the autonomic nervous system (a subcategory of dysautonomia) characterized by the onset of symptoms upon standing.
Symptoms include fatigue, lightheadedness, headache, weakness, increased heart rate/heart palpitations, anxiety, and altered vision.
[7] Often, patients have high plasma norepinephrine (NE) concentrations (at least 600 pg/ml) in relation to sympathetic outflow upon standing, suggesting OI is a hyperadrenergic condition.
[7] This discovery of the linkage with NET mutations that results in decreased norepinephrine reuptake activity and orthostatic intolerance suggests faulty NE uptake mechanisms can contribute to cardiovascular disease.
[20] Inhibition of the norepinephrine transporter (NET) has potential therapeutic applications in the treatment of attention deficit hyperactivity disorder (ADHD), substance abuse, neurodegenerative disorders (e.g., Alzheimer's disease (AD) and Parkinson's disease (PD)) and clinical depression.
[22] For many years, the number one choice in treating mood disorders like depression was through administration of TCAs, such as desipramine (Norpramin), nortriptyline (Arentyl, Pamelor), protriptyline (Vivactil), and amoxapine (Asendin).
[18] SSRIs, which mainly regulate serotonin, subsequently replaced tricyclics as the primary treatment option for depression because of their better tolerability and lower incidence of adverse effects.
Dextroamphetamine (Dexedrine, Dextrostat), Adderall, methylphenidate (Ritalin, Metadate, Concerta, Daytrana), and lisdexamfetamine (Vyvanse) block reabsorption of the catecholamines dopamine and norepinephrine through monoamine transporters (including NET), thereby increasing levels of these neurotransmitters in the brain.
The strong selective norepinephrine reuptake inhibitor (NRI), atomoxetine (Strattera), has been approved by the U.S. Food and Drug Administration (FDA) to treat ADHD in adults.
It can work to increase one's ability to focus, decrease any impulsiveness, and lessen hyperactivity in both children and adults with ADHD.
This thwarts the absorption of these chemicals into the presynaptic terminal[27] and allows a large concentration of dopamine, serotonin and norepinephrine to build up in the synaptic cleft.
Recently discovered mechanisms of the NET, including the ability to act reversibly and as an ion channel, provide other areas of research.
[32][33][34][35] The only relationship that has been understood between researchers is that there is a positive correlation between increased NE levels in the brain and spinal fluid (CSF) and activity of schizophrenia.
[32][33][34][35] In one study, clonidine, a drug used to treat medical conditions such as ADHD and high blood pressure, was shown to produce a significant decrease in plasma level MHPG (3-methoxy-4-hydroxyphenylglycol), a metabolite of NE, in the normal control group, but not in the group of schizophrenic patients.