Organ donation
Normally, nothing is done until the person has already died, although if death is inevitable, it is possible to check for consent and to do some simple medical tests shortly beforehand, to help find a matching recipient.
[13] The lead surgeon, Joseph Murray, and the nephrologist, John Merrill, won the Nobel Prize in Physiology or Medicine in 1990 for advances in organ transplantation.
[16] The oldest altruistic living organ donor was an 85-year-old woman in Britain, who donated a kidney to a stranger in 2014 after hearing how many people needed to receive a transplant.
[27] Additional concerns exist with views of compromising the freedom of choice to donate,[30] conflicts with extant religious beliefs[31] and the possibility of posthumous violations of bodily integrity.
[31] Because of public policies, cultural, infrastructural and other factors, presumed consent or opt-out models do not always translate directly into increased effective rates of donation.
[37] The president of the Spanish National Transplant Organisation has acknowledged Spain's legislative approach is likely not the primary reason for the country's success in increasing the donor rates, starting in the 1990s.
The characteristic that enables the Spanish presumed consent model to be successful is the resource of transplant coordinators; it is recommended to have at least one at each hospital where opt-out donation is practiced to authorize organ procurement efficiently.
[56] Consent for organ donation by an individual is given by either registering with the organ donation registry established by the Chambre des notaires du Québec, signing and affixing the sticker to the back of one's health insurance card, or registering with either Régie de l'assurance maladie du Québec or Registre des consentements au don d'organes et de tissus.
[58] Canadian Blood Services has a program called the kidney paired donation, where transplant candidates are matched with compatible living donors from all over Canada.
[63] Nova Scotia, Canada, is the first jurisdiction in North America to introduce an automatic organ donation program unless residents opt out; what the province refers to as deemed consent.
[65] With the legislation, all people who have been Nova Scotia residents for a minimum of 12 consecutive months, with appropriate decision-making capacity and are over 18 years of age are considered potential donors and will be automatically referred to donation programs if they are determined to be good candidates.
[76] In Italy if the deceased neither allowed nor refused donation while alive, relatives will pick the decision on his or her behalf despite a 1999 act that provided for a proper opt-out system.
The small success of Tamil Nadu model has been possible due to the coming together of both government and private hospitals, non-governmental organizations and the State Health Department.
Many Maori people believe organ donation is morally unacceptable due to the cultural need for a dead body to remain fully intact.
[117] In South Korea, the 2006 provision of the Organ Transplant Act introduced a monetary incentive equivalent to US$4,500 to the surviving family of brain-death donors; the reward is intended as consolation and compensation for funeral expenses and hospital fees.
[120] Since December 2015, Human Transplantation (Wales) Act 2013 passed by the Welsh Government has enabled an opt-out organ donation register, the first country in the UK to do so.
The Uniform Anatomical Gift Act of 1987 was adopted in several states, and allowed medical examiners to determine if organs and tissues of cadavers could be donated.
[134] Arkansas, the District of Columbia, Louisiana and Pennsylvania provide tax credits to employers for wages paid to employees on leave for organ donation.
Exploitation arguments generally come from two main areas: The New Cannibalism is a phrase coined by anthropologist Nancy Scheper-Hughes in 1998 for an article written for The New Internationalist.
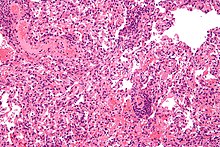
Given long enough, patients who do not fully die in the complete biological sense, but who are declared brain dead, will usually start to build up toxins and wastes in the body.
[166] That increase has provoked ethical concerns about the interpretation of "irreversible" since "patients may still be alive five or even 10 minutes after cardiac arrest because, theoretically, their hearts could be restarted, [and thus are] clearly not dead because their condition was reversible.
[170] A study published in 2022 partially explained these disparities through the higher prevalence of certain diseases in men, immune responses related to childbirth in women, and the mismatch in size between the donor and recipient.
[172] Adequate funding, strong political will to see transplant outcomes improve, and the existence of specialized training, care and facilities also increase donation rates.
Expansive legal definitions of death, such as Spain uses, also increase the pool of eligible donors by allowing physicians to declare a patient to be dead at an earlier stage, when the organs are still in good physical condition.
[citation needed] Most religions, among them the Roman Catholic Church, support organ donation on the grounds that it constitutes an act of charity and provides a means of saving a life.
"[212] Approaches to addressing this shortfall include: In hospitals, organ network representatives routinely screen patient records to identify potential donors shortly in advance of their deaths.
[221] This practice increases transplant efficiency, as potential donors who are unsuitable due to infection or other causes are removed from consideration before their deaths, and decreases the avoidable loss of organs.
[227] At California's Emanuel Medical Center, neurologist Narges Pazouki said an organ-procurement organization representative pressed her to declare a patient brain-dead before the appropriate tests had been done.
Under United States federal laws, eBay was obligated to dismiss the auction for the selling of human organs, which is punishable by up to five years in prison and a $50,000 fine.
Organ trading is banned in Singapore and in many other countries to prevent the exploitation of "poor and socially disadvantaged donors who are unable to make informed choices and suffer potential medical risks.