Pathophysiology of obesity
[3] Since this discovery, many other hormonal mechanisms have been elucidated that participate in the regulation of appetite and food intake, storage patterns of adipose tissue, and development of insulin resistance.
[4] This resistance is thought to explain in part why administration of leptin has not been shown to be effective in suppressing appetite in most obese people.
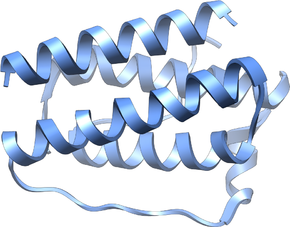
[1] While leptin and ghrelin are produced peripherally, they control appetite through their actions on the central nervous system.
In particular, they and other appetite-related hormones act on the hypothalamus, a region of the brain central to the regulation of food intake and energy expenditure.
Abdominal obesity, excess fat cell accumulation in adipose tissue of the abdomen, is associated more strongly with meta-inflammation.
[7][8][9] Excessive fat tissue has a direct effect on the productivity of the immune system by slowing it down or interrupting the activity of the cells.
It can alter the number of leukocytes, neutrophils, monocytes, and lymphocytes an individual has, while also lowering T and B cell mitogen-induced production.
The dysregulation causes apoptosis in adipose tissue cells, then activating an influx of inflammatory leukocytes, ultimately resulting in chronic inflammation.
[11] Extracellular vesicles are diminished in the adipose tissue, and they help assist in cell communication, growth, and other functions.
These hormones control metabolic functions like appetite, energy usage, and adipose tissue distribution in the body.
[12] Maintaining a healthy diet and consuming substantial nutrition will help ensure that a person has a stronger immune system.