Phenylketonuria
[1] A baby born to a mother who has poorly treated PKU may have heart problems, a small head, and low birth weight.
A baby born to a mother who has poorly treated PKU may have heart problems, a small head, and low birth weight.
[11][12] If a child is not diagnosed during the routine newborn screening test and a phenylalanine-restricted diet is not introduced, then phenylalanine levels in the blood will increase over time.
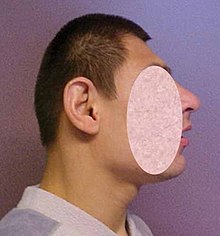
The disease may present clinically with seizures, hypopigmentation (excessively fair hair and skin), and a "musty odor" to the baby's sweat and urine (due to phenylacetate, a carboxylic acid produced by the oxidation of phenylacetone).
[13] Untreated children often fail to attain early developmental milestones, develop microcephaly, and demonstrate progressive impairment of cerebral function.
[5] PKU is characterized by homozygous or compound heterozygous mutations in the gene for the hepatic enzyme phenylalanine hydroxylase (PAH), rendering it nonfunctional.
If left untreated (and often even in treatment), complications of PKU include severe intellectual disability, brain function abnormalities, microcephaly, mood disorders, irregular motor functioning, and behavioral problems such as attention deficit hyperactivity disorder, as well as physical symptoms such as a "musty" odor, eczema, and unusually light skin and hair coloration.
Tyrosine is a conditionally essential amino acid for PKU patients because without PAH it cannot be produced in the body through the breakdown of phenylalanine.
Without dietary intervention, mild HPA patients have blood Phe levels higher than those with normal PAH activity.
As these amino acids are necessary for protein and neurotransmitter synthesis, Phe buildup hinders the development of the brain, causing intellectual disability.
[26] Recent research suggests that neurocognitive, psychosocial, quality of life, growth, nutrition, and bone pathology are slightly suboptimal even for patients who are treated and maintain their Phe levels in the target range if their diet is not supplemented with other amino acids.
[27] Classic PKU affects myelination and white matter tracts in untreated infants; this may be one major cause of neurological problems associated with phenylketonuria.
[34] Elevated levels of phenylalanine in the blood and detection of phenylketones in the urine is diagnostic, however, most patients are diagnosed via newborn screening.
[citation needed][35] PKU is commonly included in the newborn screening panel of many countries, with varied detection techniques.
[36][37] Screening for PKU is done with bacterial inhibition assay (Guthrie test), immunoassays using fluorometric or photometric detection, or amino acid measurement using tandem mass spectrometry (MS/MS).
[citation needed] The diet requires restricting or eliminating foods high in Phe, such as soybeans, egg whites, shrimp, chicken breast, spirulina, watercress, fish, nuts, crayfish, lobster, tuna, turkey, legumes, and low-fat cottage cheese.
An "exchange" system can be used to calculate the amount of Phe in a portion of food from the protein content identified on a nutritional information label.
[citation needed] Supplementary "protein substitute" formulas are typically prescribed for people with PKU (starting in infancy) to provide the amino acids and other necessary nutrients that would otherwise be lacking in a low-phenylalanine diet.
Its use is limited in the US due to the cost but is available in most countries as part of a low protein / PHE diet to replace missing nutrients.
[citation needed] Furthermore, CGMP contains a high amount of the Phe-lowering LNAAs, which constitutes about 41 g per 100 g protein[45] and will therefore help maintain plasma Phe levels in the target range.
[50] Though the developing fetus may only be a carrier of the PKU gene, the intrauterine environment can have very high levels of phenylalanine, which can cross the placenta.
This is achieved by performing regular blood tests and adhering very strictly to a diet, in general, monitored on a day-to-day basis by a specialist metabolic dietitian.
In many cases, as the fetus' liver begins to develop and produce PAH normally, the mother's blood Phe levels will drop, requiring an increased intake to remain within the safe range of 2–6 mg/dL.
When maternal blood Phe levels fall below 2 mg/dL, anecdotal reports indicate that the mothers may experience adverse effects, including headaches, nausea, hair loss, and general malaise.
A 1987 study from Slovakia reports a Roma population with an extremely high incidence of PKU (one case in 40 births) due to extensive inbreeding.
Nobel and Pulitzer Prize-winning author Pearl S. Buck had a daughter named Carol who lived with PKU before treatment was available, and wrote an account of its effects in a book called The Child Who Never Grew.
[62] Phenylketonuria was discovered by the Norwegian physician Ivar Asbjørn Følling in 1934[63] when he noticed hyperphenylalaninemia (HPA) was associated with intellectual disability.
He conducted tests and found reactions that gave rise to benzaldehyde and benzoic acid, which led him to conclude that the compound contained a benzene ring.
[65] In 1954, Horst Bickel, Evelyn Hickmans and John Gerrard published a paper that described how they created a diet that was low in phenylalanine and the patient recovered.
In February 2022, the FDA issued a statement requiring further data from non-clinical studies to assess oncogenic risk resulting from PEG-PAL treatments.