Post-traumatic seizure
[2] Thus, people who sustain severe head trauma are given anticonvulsant medications as a precaution against seizures.
The risk that a person will develop PTS becomes progressively lower as time passes after the injury.
[14] Early PTS are considered to be provoked seizure, because they result from the direct effects of the head trauma and are thus not considered to be actual epilepsy, while late seizures are thought to indicate permanent changes in the brain's structure and to imply epilepsy.
[14] Factors that may result in seizures that occur within two weeks of an insult include the presence of blood within the brain; alterations in the blood brain barrier; excessive release of excitatory neurotransmitters such as glutamate; damage to tissues caused by free radicals; and changes in the way cells produce energy.
[13] Medical personnel aim to determine whether a seizure is caused by a change in the patient's biochemistry, such as hyponatremia.
[4] For example, a 2003 review of medical literature found phenytoin to be preventative of early, but probably not late PTS.
[4] For unknown reasons, prophylactic use of antiepileptic drugs over a long period is associated with an increased risk for seizures.
[1] For these reasons, antiepileptic drugs are widely recommended for a short time after head trauma to prevent immediate and early, but not late, seizures.
[13] Antiepileptic drugs that may be given intravenously shortly after injury include phenytoin, sodium valproate, carbamazepine, and phenobarbital.
[14] It is unknown exactly how long after a TBI a person is at higher risk for seizures than the rest of the population, but estimates have suggested lengths of 10 to over 15 years.
[5] The likelihood that PTS will go into remission is lower for people who have frequent seizures in the first year after injury.
[12] Research has found that the incidence of PTS varies widely based on the population studied; it may be as low as 4.4% or as high as 53%.
[9] The most important factor in whether a person will develop early and late seizures is the extent of the damage to the brain.
[2] More severe brain injury also confers a risk for developing PTS for a longer time after the event.
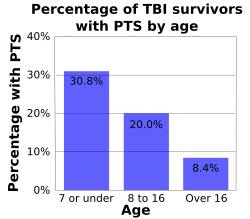
[5][22] Early seizures occur up to twice as frequently in brain injured children as they do in their adult counterparts.
[11] One study found the incidence of early seizures to be highest among infants younger than one year and particularly high among those who sustained perinatal injury.
[2] If a fragment of metal remains within the skull after injury, the risk of both early and late PTS may be increased.
[5] Head trauma survivors who abused alcohol before the injury are also at higher risk for developing seizures.
[9] PTA that lasts for longer than 24 hours after the injury is a risk factor for both early and late PTS.