Poverty and health in the United States
[7][8] According to Unhealthy Cities: Poverty, Race, and Place in America, poor air quality results in higher rates of children with asthma living in these areas, and nearly 2 million children with asthma live in areas that do not meet national ozone standards.
[8] Low-income populations are also more exposed to pesticides, and a significantly higher amount of lead was found in African-American children living in inner-city areas.
[11] From air pollution, respiratory and cardiovascular diseases can worsen due to the greater amounts of chemicals in the atmosphere and hotter temperatures.
[12] For those living in rural areas, health services are not as accessible, and impoverished people go to doctors fewer times than their counterparts.
Research has shown that low-income families and their children face the most pressing struggles when it comes to receiving medical attention.
Since its most recent reauthorization in 2018, the Children’s Health Insurance Program (CHIP) aims at improving healthcare coverage for vulnerable families experiencing homelessness.
[13] The initiatives for youth, as well as the automatic enrollment at birth, together represent a significant step towards enhancing effective health care access for families in this population.
Previous research has identified the labor environments of the impoverished as more likely to contain risk factors for illness and disability relative to their non-impoverished counterparts.
Housing is what the poor pay the most for on a regular basis, and this results in lack of funds for other basic needs like food and health.
[7][17][19] In a National Health Interview Survey, it was found that around 10% of American families did not receive needed medical care because of cost.
[5][6] After the 1980s decision to close long-term mental health-focused residential facilities, individuals suffered without adequate support systems and without access to community-based services.
[22] These individuals experienced unemployment, homelessness, and exposure to the criminal justice system, further exacerbating their mental illness.
Schizophrenia is also strongly associated with poverty, occurring most frequently in the poorest classes of people all over the world, especially in more unequal countries.
[24] With those in poverty having a greater likelihood of suffering from mental illness, the benefit of access to clinical psychotherapy treatments has been explored.
[16] When compared to White Americans, all other races have lower outcomes of infant mortality, low birth weight, prenatal care, and deaths in cities.
[7] Most current neighborhoods that are predominantly Black have been institutionally disinvested and have fewer public services and more housing insecurity.
[27] These adverse health consequences are associated with poor living conditions and a lack of access to treatment facilities.
Without it, individuals and families are left to deal with their ailments themselves or endure further financial burden by receiving treatments without a health insurance plan.
[28] The close living spaces of areas such as Skid Row in California provide an environment in which infectious diseases can spread easily.
Conversely, homelessness can cause further health issues, due to constant exposure to environmental threats such as violence and communicable diseases.
Homeless people have disproportionately high rates of poly substance use, mental illness, physical health problems and legal issues/barriers in attaining employment.
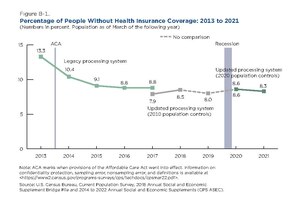
[36] Insurance tends to increase the price of services,[9] and at that time, 8.5% of people belonging to households that made over $75,000 annually were uninsured.
While these positive effects were observed, outcomes for heart disease, diabetes, and other physical health characteristics were not meaningfully improved.
It has been posited that one year, the duration of the study, is an insufficient length to fully observe the divergent health outcomes that would be characteristic of an experiment with a lengthier timetable.
Unhoused individuals often struggle to provide such documentation, or they may not meet the standards and income thresholds, thus limiting their access to Medicaid and the essential healthcare services that follow.
[40] The Affordable Care Act was passed in 2010, and it expanded Medicaid eligibility and provided funding for federally qualified health centers.
Another idea is to implement community-oriented primary care where physicians consider the environment and culture of the patient to further their health.
[41][42][43] Policy wise, it is recommended to continue investing in the health of the poor by creating an amendment or law and increasing affordable housing.