Plasmid-mediated resistance
[3] Plasmids often carry multiple antibiotic resistance genes, contributing to the spread of multidrug-resistance (MDR).
[4] Antibiotic resistance mediated by MDR plasmids severely limits the treatment options for the infections caused by Gram-negative bacteria, especially family Enterobacteriaceae.
[7] They are frequently accompanied by the genes encoding virulence determinants,[8] specific enzymes or resistance to toxic heavy metals.
[citation needed] They were first found in Japan in 1959 when it was discovered that some Shigella strains had developed resistance to a number of antibiotics used to treat a dysentery epidemic.
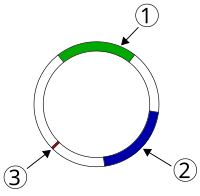
[citation needed] Bacteria containing F-factors (said to be "F+") have the capability for horizontal gene transfer; they can construct a sex pilus, which emerges from the donor bacterium and ensnares the recipient bacterium, draws it in,[16] and eventually triggers the formation of a mating bridge, merging the cytoplasms of two bacteria via a controlled pore.
[23] Members of family Enterobacteriaceae, for example, Escherichia coli or Klebsiella pneumoniae pose the biggest threat regarding plasmid-mediated resistance in hospital- and community-acquired infections.
Often multiple beta-lactamase genes are found on the same plasmid hydrolyzing a wide spectrum of beta-lactam antibiotics.
The first clinically observed ESBL enzymes were mutated versions of the narrow spectrum beta-lactamases, like TEM and SHV.
Carbapenemases represent type of ESBL which are able to hydrolyze carbapenem antibiotics that are considered as the last-resort treatment for ESBL-producing bacteria.
[28] The qnr genes can be discovered in integrons and transposons on MDR plasmids of various incompatibility groups, which could carry a number of resistance-related molecules, such as carbapenemases and ESBLs.
[29] Examples of resistance mechanisms include different Qnr proteins, aminoglycose acetyltransferase aac(6')-Ib-cr that is able to hydrolyze ciprofloxacin and norfloxacin, as well as efflux transporters OqxAB and QepA.
[5] xResistance to aminoglycosides in Gram-negative pathogens is primarily caused by enzymes that acetylate, adenylate, or phosphorylate the medication.
These sRNAs were antisense to genes involved in replication, conjugate transfer and plasmid stabilisation : AS-repA3 (CopA), AS-traI, AS-finO, AS-traG, AS-pc02 .