Spectrum disorder
A spectrum approach may also expand the type or the severity of issues which are included, which may lessen the gap with other diagnoses or with what is considered "normal".
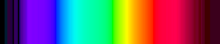
Isaac Newton first used the word spectrum (Latin for "appearance" or "apparition") in print in 1671, in describing his experiments in optics.
The term was first used by analogy in psychiatry with a slightly different connotation, to identify a group of conditions that is qualitatively distinct in appearance but believed to be related from an underlying pathogenic point of view.
It has been noted that for clinicians trained after the publication of DSM-III (1980), the spectrum concept in psychiatry may be relatively new, but that it has a long and distinguished history that dates back to Emil Kraepelin and beyond.
These categories are aids important for our practical purposes such as providing specific labels to facilitate payments for mental health professionals.
For example, a model that was derived from linguistic expressions of individual differences is subdivided into the Big Five personality traits, where everyone can be assigned a score along each of the five dimensions.
Similarly, in the classification of mental disorders, a dimensional approach, which is being considered for the DSM-V, would involve everyone having a score on personality trait measures.
This identifies a significant amount of symptoms and impairment below threshold for DSM diagnosis but nevertheless important, and potentially also present in other disorders a person might be diagnosed with.
[15] An autistic spectrum[16] – in its simplest form this joins autism and Asperger syndrome, and can additionally include other pervasive developmental disorders (PDD).
[24] Other spectrum approaches include more specific individual phenomena which may also occur in non-clinical forms in the general population, such as some paranoid beliefs or hearing voices.
[25] Some researchers have also proposed that avoidant personality disorder and related social anxiety traits should be considered part of a schizophrenia spectrum.
A spectrum approach joins these together and may additionally include specific clinical variables and outcomes, which initial research suggested may not be particularly well captured by the different diagnostic categories except at the extremes.
On the one hand, work on major depressive disorder has identified a spectrum of subcategories and sub-threshold symptoms that are prevalent, recurrent and associated with treatment needs.
[33] In addition, numerous subtypes of bipolar have been proposed beyond the types already in the DSM (which includes a milder form called cyclothymia).
These extra subgroups have been defined in terms of more detailed gradations of mood severity, or the rapidity of cycling, or the extent or nature of psychotic symptoms.
[clarification needed] Paraphilic behavior is triggered by thoughts or urges that are psychopathologically close to obsessive impulsive area.
In the last case, the pleasure gained is short in time and is followed by a new increase in anxiety levels, such as it can be seen in an obsessive patient after he performs his compulsion.
[1] One psychological model based on factor analysis, originating from developmental studies but also applied to adults, posits that many disorders fall on either an "internalizing" spectrum (characterized by negative affectivity; subdivides into a "distress" subspectrum and a "fear" subspectrum) or an "externalizing" spectrum (characterized by negative affectivity plus disinhibition).
From a psychological point of view, it has been suggested that the underlying phenomena are too complex, inter-related and continuous – with too poorly understood a biological or environmental basis – to expect that everything can be mapped into a set of categories for all purposes.
In this context the overall system of classification is to some extent arbitrary, and could be thought of as a user interface which may need to satisfy different purposes.